Visual Impairment Linked to Increased Dementia Risk in Aging Women
An analysis from the Women's Health Initiative has uncovered a potential link between visual impairment and risk of incident dementia.
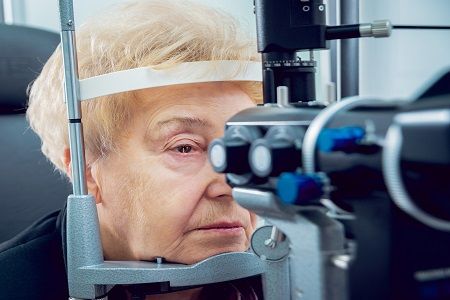
New data Byers Eye Institute at Stanford University suggests the presence of visual impairment could help predict risk of incident dementia in older women.
A secondary analysis including 1061 women, the study also revealed the severity of visual impairment appeared to correlate with an increased risk of dementia in the study cohort.
Using information form the Women’s Health Initiative (WHI), which included more than 160k women, a team led by Suzann Pershing, MD, MS, sought to evaluate potential associations between visual impairment and risk of cognitive impairment. Women included in the current study participated in the WHI Sight Examination (WHISE) and WHI Memory Study (WHIMS).
After exclusion of those with baseline cognitive impairment and those who did not have complete information related to analysis variables, investigators were left with a cohort of 1061 patients. For the purpose of their study, investigators defined visual impairment using visual acuity and questionnaires.
A total of 3 thresholds were established to define visual acuity: nonpinhole visual acuity of 20/40 or worse, 20/80 or worse, and 20/100 or worse in at least 1 eye. The primary outcome of the analysis was indecent probable dementia. Investigators noted additional evaluation for incident mild cognitive impairment (MCI), with or without progress to dementia, and a composite of incident cases of probable dementia or first MCI.
In total, 12 regression models were used in the current analysis, all of which were adjusted for confounder including age, race/ethnicity, smoking status, systemic comorbidities, and hormone therapy trial arm.
Of the 1061 women included in the study, which had a mean age of 73.8 years at baseline, 206 had self-reported visual impairment and 183 had objective visual impairment of 20/40 or worse. Over a median follow-up of 3.8 years, 42 (4.0%) women were classified with probable dementia and 28 (2.6%) women were classified as having MCI that did not progress to dementia.
Upon analysis, results indicated risk of dementia was greater among women with visual impairment than those without and this association became greater with worsening vision. Hazard ratios indicated risk of incident dementia was 5.66-fold greater among those with visual acuity of 20/100 or worse (HR, 5.66; 95% CI, 1.75-18.37), 5.2-fold in those with 20/80 vision or worse (HR, 5.20; 95% CI, 1.94-13.95), and 2.14-fold in those with 20/40 vision or worse (HR, 2.14; 95% CI, 1.08-4.21).
When examining risk for MCI, those with baseline visual acuity of 20/100 or worse were at the greatest risk (HR, 6.43; 95% CI, 1.66-24.85). Of note, investigators indicated age was the only variable associated with dementia or MCI, but patients who reported both visual impairment and self-reported hearing loss had an even greater risk of developing dementia.
An additional analysis sought to determine whether presence of specific ocular disease, such as age-related macular degeneration, was associated with increased risk of incident dementia. Results of the study indicated some conditions were associated with increased risk in unadjusted models but they failed to reach statistical significance and none were associated with dementia after adjustment for confounders.
Investigators pointed out the study had multiple limitations including the observational nature of the analysis, which limit the applicability of their study. Other limitations included only assessing visual impairment through visual acuity and the WHI Hormone Therapy Clinical Trials enrolling women who fit specific eligibility criteria.
This study, “Association of Visual Impairment With Risk of Incident Dementia in a Women’s Health Initiative Population,” was published online in JAMA Ophthalmology.