Wet AMD: Ranibizumab to Aflibercept Switch Does Not Improve Visual Acuity in Poor-Responders
Suleyman Kaynak, MD, and colleagues from the Dokuz Eylul University in Turkey, evaluated an alternative therapy for patients who do not respond well to intravitreal ranibizumab.
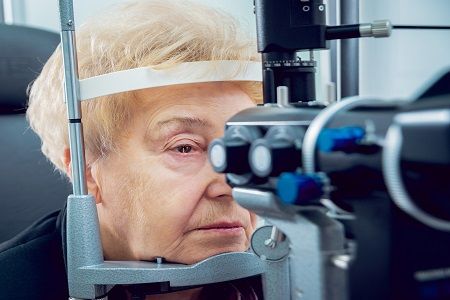
Patients respond differently to treatments, and if a response is less than desirable, it’s time to choose a plan B. Intravitreal ranibizumab is one treatment option for people with wet age-related macular degeneration (AMD), but Suleyman Kaynak, MD, and colleagues from the Dokuz Eylul University in Turkey, evaluated an alternative therapy for patients who do not respond well to it.
In a poster session presented at the 34th Annual Scientific Meeting of the American Society of Retina Specialists (ASRS 2016) in San Francisco, California, the team revealed outcomes with intravitreal aflibercept after patients did not respond to intravitreal ranibizumab well.
- MD Magazine is on Facebook, Twitter, Instagram, and LinkedIn!
The analysis included 33 eyes with wet AMD. The participants were classified as poor-responders — categorized after six months or more of intravitreal ranibizumab treatment. Monthly examinations included best corrected visual acuity (BCVA) assessment, dilated fundoscopy, and spectral domain optical coherence tomography (SD-OCT) evaluation. In addition, fluorescein angiography (FA) was performed before ranibizumab injections, during the drug switching period, and any imperative conditions.
The participants, with an average age of nearly 70, had a mean follow-up of 33.8 months. On average, 2.2 aflibercept injections were given to the cohort after first trying about eight ranibizumab injections.
“Intravitreal aflibercept injections in wet AMD cases who were poor responder to previous ranibizumab treatment provide good anatomical success,” the authors concluded. “However any significant improvement in visual acuity was not gained after drug switching.”
BCVA (logMAR) scores averaged at 0.42 at baseline, 0.45 at the time of drug switching, and 0.46 at their last visit. CMT (µm) moved from 404 at baseline, 395.8 at drug switching, and 300.9 at their last visit.
Also on MD Magazine >>> More News from ASRS 2016 in San Francisco