The 10-minute examination for low back pain
Low back pain (LBP) is a major public health problem and a common reason for patient visits to a primary care physician. A pathoanatomically precise diagnosis cannot be made in most patients, and the primary care physician typically has only limited time to conduct a complete examination. A brief visit that is highly structured for efficiency can provide direction about the underlying pathology of acute LBP, leading to appropriate pharmacotherapy and adjunctive measures. Asking targeted questions during the history taking is the key to a successful diagnosis. Patient education helps ensure a successful outcome. Use of analgesics and skeletal muscle relaxants can help relieve symptoms in many patients. (J Musculoskel Med. 2008;25:162-168).
ABSTRACT: Low back pain (LBP) is a major public health problem and a common reason for patient visits to a primary care physician. A pathoanatomically precise diagnosis cannot be made in most patients, and the primary care physician typically has only limited time to conduct a complete examination. A brief visit that is highly structured for efficiency can provide direction about the underlying pathology of acute LBP, leading to appropriate pharmacotherapy and adjunctive measures. Asking targeted questions during the history taking is the key to a successful diagnosis. Patient education helps ensure a successful outcome. Use of analgesics and skeletal muscle relaxants can help relieve symptoms in many patients. (J Musculoskel Med. 2008;25:162-168)
Acute painful musculoskeletal symptoms are commonplace in primary care, and low back pain (LBP) is the most frequently reported subcategory. In fact, acute LBP is one of the most common reasons why patients visit a primary care clinician. LBP is a major public health problem that decreases quality of life and increases health care costs. Patients may become significantly restricted in their activities; low back problems are the most common cause of disability in persons younger than 45 years.1
The history taking and physical examination usually allow for categorization of LBP, and conservative treatment often is effective in relieving symptoms and returning patients to activity. For most patients, however, a discrete pathological entity causing LBP is not identifiable. Rather, the job of the clinician is to detect secondary causes of back pain (eg, disk space infection, ankylosing spondylitis, or primary or metastatic neoplasia); confirm the absence of LBP requiring urgent intervention (eg, cauda equina syndrome); and expeditiously manage the remaining vast majority of patients with LBP, who can be aptly grouped as having mechanical LBP. A precise diagnosis cannot be made for more than 85% of patients presenting with LBP.2 However, a competent targeted examination generally is adequate to attain these goals.
Busy primary care physicians can find an answer to this vexing problem in the 10-minute examination for LBP. This quick, effective approach to diagnosis and management promotes efficiency and improves the chances of a successful outcome by combining an element of structure with simultaneous, targeted questions and patient education. A highly structured visit such as this helps physicians quickly discern between patients who can be treated conservatively with short-term pharmacotherapy and consideration of physical therapy and those who require more aggressive investigation and treatment. Ultimately, a small percentage of patients with LBP (typically fewer than 5%) will require referral for specialty care. In this article,we outline the simple steps to take in this approach.
Background and anatomy
Knowledge of the anatomy is useful for making the diagnosis and providing appropriate treatment. The spine is a complex structure that protects the spinal cord and transfers loads from the head and trunk to the pelvis. Each vertebra articulates with adjacent ones to permit motion in 3 planes. Intrinsic stability is gained from the intervertebral disks and surrounding ligaments, and extrinsic support comes from the surrounding muscles.
The lumbar spine is composed of 5 vertebrae, each consisting of a body anteriorly and a neural arch posteriorly that encloses the vertebral canal. The spinal cord and cauda equina pass through, protected by the structures surrounding the canal.
The neural arch has 2 pedicles on its sides and a lamina posteriorly.A spinous process projects posteriorly from the lamina in the midline; a transverse process projects laterally from each side at the junction of the pedicle and lamina.
There are 2 categories of LBP. Primary, or mechanical, LBP (also known as nonspecific LBP) is any pain not associated with a secondary underlying pathology. It typically persists for less than 3 weeks and usually results from an acknowledged precipitating event. Most patients describe a physical activity (often trivial) that induced the pain; stepping off a curb, sneezing, coughing, or twisting may have precipitated significant symptoms. Secondary LBP is that produced by an identifiable underlying pathology, such as neoplasia, aortic aneurysm, or disk space infection.
The first 5 minutes
To conduct an effective back examination in 10 minutes,you will need to be prepared to move with brisk direction from introductions to history taking to physical examination to counseling and closeout. In most cases, a brief and focused history provides more information to arrive at a diagnosis than does the physical examination. You may wish to have a list of the necessary questions ready in advance (Table 1); they can be administered by direct interview or even by offering a questionnaire before the interview.
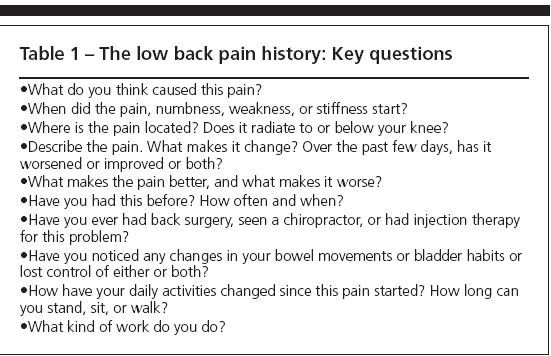
Table 1
Characterization of the patient's pain should include its time of onset, a description (eg, burning, lancinating, or boring), factors that exacerbate or alleviate, radiation, and its time course during the day (eg, worsens at night, worsens with activity, or worsens with sitting or standing). Attention should be paid to the patient's perception of pain, including its nature and intensity.
Accrediting organizations now emphasize pain management and assessment in a manner that suggests a fifth vital sign. Verbal, visual, and pictorial pain scale tools can guide the patient's comments efficiently and provide excellent records in the patient's own words.3 Ask the patient to describe how the pain has altered his or her activities and to document this description clearly and concisely.
Recognizing red flags
At this point, try to screen out patients who have conditions that are more complicated than an acute mechanical type of LBP. Fewer than 2% of patients with LBP present with significant neurological involvement or other signs that mandate imaging or referral or both.4 Several signs in patients with LBP that suggest consideration of investigation for secondary causes or radiographic evaluation are listed in Table 2; these findings may suggest infection, malignancy, or serious neurological involvement.
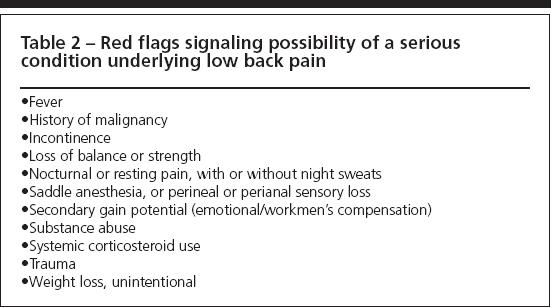
Table 2
For acute LBP, radiographic studies rarely are useful unless a fracture or other secondary pathology is suspected. More often than not, early radiographic findings actually muddy the clinical waters, because clinical trials have shown that many asymptomatic healthy young adults have findings on CT scans or MRI that are consistent with disk pathology. Similarly, the absence or presence and severity of osteoarthritic change on x-ray films do not correlate with clinical findings.
In uncomplicated acute LBP, clinicians may consider imaging if symptoms do not improve after a good therapeutic trial (usually at least 4 to 6 weeks of conservative treatment), unless the condition does not improve after 5 to 6 or more weeks.3 Radiographic studies also are needed if more complicated issues are suspected at the following visit.
Plain x-ray films are useful only when secondary pathology, such as neoplasia, is sought. Advanced radiography, such as MRI or CT, should be used only in refractory cases (pain that persists after 8 to 12 weeks), in patients who have progressively worsening symptoms or neurological deficit, and when surgical intervention is planned.
A time-efficient examination
Now the patient is ready for a quick 4-part physical examination: gait observation, regional palpation, mechanical range of motion, and strength testing. Whether to ask the patient to disrobe entirely or remove only his upper garments and loosen his lower garments can be guided by your preliminary assessment of the severity of the problem. Having the patient undressed and comfortably gowned before going in can help save time.
Gait observation. Observe the patient's gait as he rises and moves to the examining table to determine whether it is shortened, asymmetrical, or antalgic (accompanied by facial pain signs or pain behaviors, such as guarding or grimacing).3 Also note any foot drop; any neurological deficit can indicate a potentially more serious problem.3 If the distance from your desk to the examination area is very short, ask the patient to walk in the hallway to gain a better observation.
Palpation.This should be gentle; major manipulation should not be needed to find pain or tenderness. Look for trigger points and radiation of pain. Saddle anesthesia is a cardinal sign of cauda equina syndrome; this merits urgent referral for definitive surgical care.
Range of motion. Sciatic nerve compression is assessed easily using the straight-leg raising test (Figure 1). The results are considered abnormal if pain is elicited or worsened with elevation of the leg higher than 25° but lower than 75°.1 The pain must radiate below the knee for the test result to be considered positive for sciatica; limitation of range of motion may be the result of hamstring tightness rather than disk pathology.
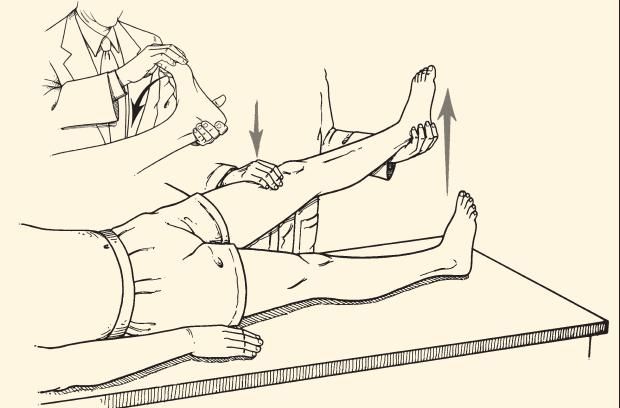
In the straight-leg raising test, the patient lies on a table in the supine position. With one hand placed above the knee of the leg being examined, the examiner exerts enough firm pressure to keep the knee fully extended. With the other hand cupped under the heel, the examiner raises the straight limb slowly. Sciatic nerve compression is indicated if pain is elicited or worsened on elevation of the leg higher than 25° but lower than 75º. The ankle is dorsiflexed as the leg is held at the limit of straight-leg raising (inset). Symptoms are exacerbated in persons who have nerve root compression as the cause.
Pain elicited when the patient's leg is elevated less than 25° is inconsistent with known pathology and may indicate that other issues, such as symptom magnification, are present. At the point in the straight-leg examination when pain is produced, foot dorsiflexion should exacerbate symptoms in persons with nerve root compression as the cause. If foot dorsiflexion does not intensify pain, a tight hamstring is more likely the cause.
In the crossed-leg examination, performing the procedure on the contralateral leg produces pain (ie, raising the right leg produces left-sided pain) that may be indicative of a large midline disk lesion.This test is more specific than the standard straight-leg raising test but less sensitive.
Now, ask the patient to stand and flex forward. Document how far he can flex forward without bending his knees while attempting to touch his toes. Measure the distance from fingertips to floor; this is a quantitative measure for comparison at the next visit. Place your hand in the small of his back and ask him to slowly extend backward. Note verbal or facial expressions indicating pain or limited motion and whether the patient deviates to the left or right or exhibits guarding behavior.
Strength testing. Ask the patient to walk a few steps on his toes and then on his heels (Figure 2). Inability to toe walk indicates S1 root nerve damage; inability to heel walk may indicate L4 or L5 involvement. If the patient cannot heel walk, ask him to squat-inability to do so indicates L4 problems.1
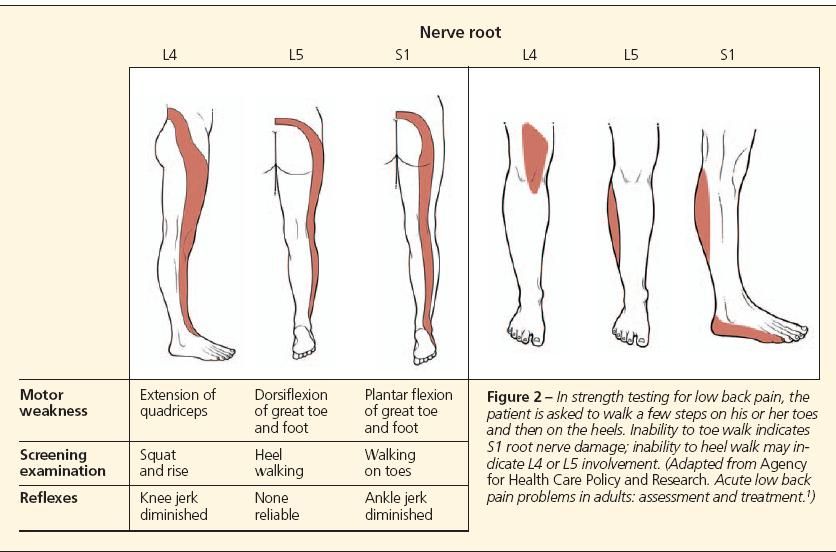
In strength testing for low back pain, the
patient is asked to walk a few steps on his or her toes
and then on the heels. Inability to toe walk indicates
S1 root nerve damage; inability to heel walk may indicate
L4 or L5 involvement. (Adapted from Agency
for Health Care Policy and Research. Acute low back
pain problems in adults: assessment and treatment.1)
Nonphysiological physical responses should alert the clinician to potential problems with symptom magnification or even frank malingering. These responses may include exaggerated pain response to light palpation, lack of pain when distracted, nonreproducibility of pain (eg, negative straight-leg raising test result when patient is seated but positive result with lying down), and pain produced by stress on noninvolved tissues (eg, pressure on the top of the head or rotation of the torso producing increased LBP).
Patient education
Patients who experience acute LBP often fear serious, progressive, or debilitating consequences. Maintaining a positive attitude helps alleviate patient fears. Consider mentioning that, in most cases, acute LBP resolves within days to weeks without long-term sequelae. Localized LBP pain, in the absence of bladder or bowel changes or other indicators of secondary disease, should be reassuring to both the clinician and the patient. It may take more than one message about the likely favorable outcome of acute LBP to convince the reluctant or apprehensive patient. Basic advice may include the following:
- Ice can be applied for 15 to 20 minutes 4 to 6 times in a 24-hour period. Warn patients that applying ice directly to skin can cause burns; it should be wrapped in a towel or some barrier between the ice and the skin should be in place. After 24 hours, ice and heat can be alternated for 20 minutes every 3 to 4 hours (warn against excessive application of heat, which can result in burns).
- Advise a commonsense approach to ergonomic and postural issues.
- Point out that patients who stay the most active enjoy the most rapid recovery. Direct patients to avoid activities that clearly worsen pain but to continue to be as active as possible. Progressive exercise generally is fully acceptable within the first 72 to 96 hours after the onset of acute LBP.
- Sleeping flat on the back with a pillow beneath the knees or sleeping on the side with the top leg flexed on a pillow or with a pillow between the legs may enhance comfort for some patients.
Pulling out the prescription pad
Many patients want and need adjunctive treatment. Analgesics (usually traditional NSAIDs) and skeletal muscle relaxants can enhance mobilization and comfortable return to activity during the natural recuperative period.
Analgesics. Either acetaminophen or any of the NSAIDs usually offer adequate short-term relief.5-7 If pain is more intense than would be anticipated to respond adequately to these measures, more potent analgesics may be used as "rescue medication" for short periods (less than 3 weeks). Cost, dose frequency, and tolerability influence the selection.7,8 Scheduled, by-the-clock dosing can interrupt a cycle of pain and increase the likelihood of success; emphasize to patients that they should take analgesics before the pain becomes intense.
Both NSAIDs and skeletal muscle relaxants have been shown to reduce the duration of symptoms. It also has been determined that the mechanism of action of muscle relaxants is independent of sedation.
NSAIDs and, more recently, the cyclooxygenase-2 (COX-2) inhibitors often mainly are used to manage both pain and inflammation. Both classes of agents appear to provide analgesia principally through inhibition of peripheral inflammation, although central mechanisms may play an important role.
Celecoxib appears to improve pain and decrease inflammation to the same degree as traditional NSAIDs. Selective COX-2 inhibitors cause fewer GI problems (dyspepsia, abdominal pain, and nausea) than the older nonselective NSAIDs.
Topical medications, such as lidocaine patches and topical diclofenac, also may provide adequate analgesia. Both formulations obviate the potential toxicity seen with systemic therapies.
The pain may be severe enough to warrant short-term, sustained use of an opioid analgesic. Agents in Schedules III and IV generally are strong enough to offer short-term relief.9 All have similar pharmacological profiles; they should be increased until analgesia is obtained. However, the use of opioid analgesics in chronic noncancer pain continues to be controversial.
There is a conspicuous lack of evidence to indicate that chronic opioid therapy improves functional outcome for patients with LBP. Therefore, the authors generally do not advocate its use. However, for hyperacute LBP-the phase of marked intensity where a patient may be immobilized by pain, unable to move or straighten up, or even unable to get up on the examining table-it is reasonable to use short-term opioid analgesia (48 to 72 hours).
Skeletal muscle relaxants. Several studies have reported that the combination of skeletal muscle relaxants and NSAIDs is superior to NSAIDs alone in treating patients with LBP.10-13 These agents often are classified by their similarities to or derivation from benzodiazepines, tricyclic antidepressants, antihistaminics, sedative/hypnotics, and alpha2-agonists (tizanidine). Because there are few head-to-head trials, stratifying agents by efficacy is not possible. Patients who previously have had LBP may ask for a muscle relaxant.
Benzodiazepines usually are not considered first-line agents for LBP. If needed, they should be selected with attention to their varying durations of action. Diazepam is the only benzodiazepine approved by the FDA for the treatment of patients with LBP resulting from muscle spasm.
Some clinical scenarios (eg, trauma) invite capitalizing on the sedative impact seen with methocarbamol, carisoprodol, cyclobenzaprine, and other agents. Most patients prefer not to be sedated, but newer skeletal muscle relaxant formulations (lower doses and extended-release products) provide for a reduced incidence of and less intense sedation. Avoidance of sedation with skeletal muscle relaxants increases the likelihood of rapid, unimpaired return to full, normal activity.
Related issues of importance to the patient are acuity level (working) and driving. Although few patients with acute LBP require any bed rest, if it is used, 2 days has been shown to be as efficacious as 7 days; protracted leave from work should be the exception rather than the rule. Driving depends on whether a sedating medication is used. Good counsel might be to avoid driving; advise patients that driving risk is increased before awareness of impairment is present.
Most acute LBP shows a trend toward improvement within 3 to 4 days. Patients with more persistent symptoms may be offered physical therapy, chiropractic or osteopathic manual medicine techniques, or a combination.
Scheduling follow-up
All patients should be counseled to call you if the problem worsens or does not improve within 48 to 72 hours after following your advice. Ask them to return within 3 to 14 days, depending on your assessment. Do not put the appointment too far in the future; doing so may lead to the perception that you are not concerned.
Patients with LBP usually enjoy a rapid restoration of functional capacity. Persons who demonstrate persistent or progressive symptoms merit further investigation or intervention. However, these are a minority of persons with LBP.
References:
References
- Agency for Health Care Policy and Research. Acute low back pain problems in adults: assessment and treatment. www. chirobase.org/07Strategy/AHCPR/ahcprclinician. html. Accessed March 11, 2008.
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363-370.
- Cohen R, Chopra P, Upshur C. Primary care work-up of acute and chronic symptoms. Geriatrics. 2001;56:26-37.
- Spitzer WO, LeBlanc FE, Dupuis M, et al; Quebec Task Force on Spinal Disorders. Scientific approach to the assessment and management of activity-related spinal disorders: a monograph for clinicians. Spine. 1987;12(suppl 1):51-59.
- Cohen RI, Chopra P, Upshur C. Guide to conservative, medical, and procedural therapies.Geriatrics. 2001;56:38-47.
- Curatolo M, Bogduk N. Pharmacologic pain treatment of musculoskeletal disorders: current perspectives and future prospects. Clin J Pain. 2001;17:25-32.
- Van Tulder MW, Scholten RJ, Koes BW, Deyo RA. Nonsteroidal anti-inflammatory drugs for low back pain. Spine. 2000;25:2501-2513.
- Coste J, Delecoeuillerie G, Cohen de Lara A, et al. Clinical course and prognostic factors in acute low back pain: an inception cohort study in primary care practice. BMJ. 1994;308:577-580.
- Curtis P, Carey TS, Evans P, et al. Training in back care to improve outcome and patient satisfaction: teaching old docs new tricks. J Fam Pract. 2000;49:786-792.
- Basmajian JV. Acute back pain and spasm: a controlled multicenter trial of combined analgesic and antispasm agents. Spine. 1989;14:438-439.
- Berry H, Hutchinson DR. Tizanidine and ibuprofen in acute low-back pain: results of a double-blind multicentre study in general practice. J Int Med Res. 1988;16:83-91.
- Borenstein DG, Lacks S, Wiesel SW. Cyclobenzaprine and naproxen versus naproxenalone in the treatment of acute low back pain and muscle spasm. Clin Ther. 1990;12:125-131.
- Cherkin DC, Wheeler KJ, Barlow W, Deyo RA. Medication use for low back pain in primary care. Spine. 1998;23:607-614.