An 11-Year-Old Haitian Male with Left Leg Pain
A combination of Gaucher's disease and sickle cell anemia in an 11-year-old boy presenting with leg pain may have been the secret to his survival for more than 28 years.
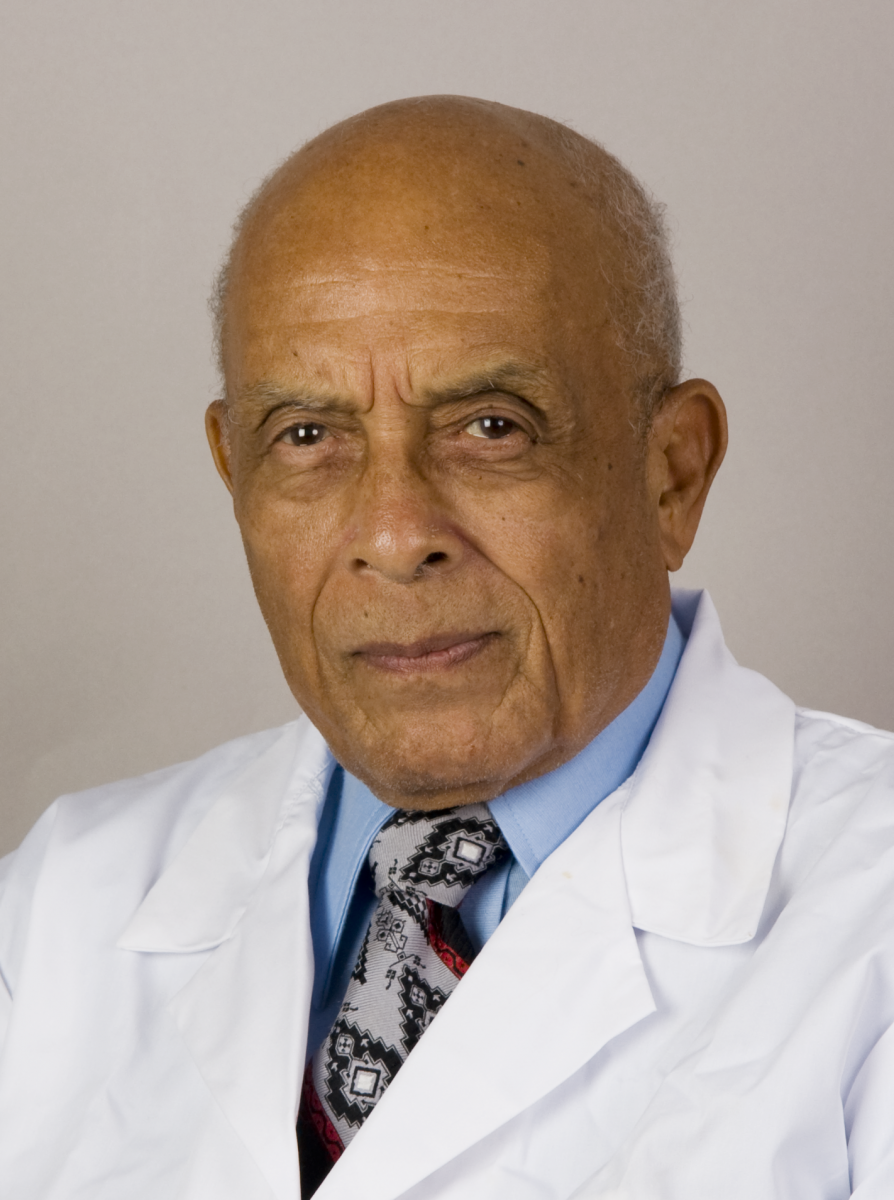
James D. Collins, MD
An 11-year-old Haitian boy who lives with his parents at a high altitude presented with a chief complaint of bone pain in his left leg after exercising. His complaint of pain began 3 months prior to his clinical evaluation. The patient’s mother indicated that she has sickle cell trait and his father has Gaucher’s disease. The boy’s pediatrician detected palpable pain over the left knee, so an anterior-posterior (AP) X-ray was obtained over that area.
Radiographic Findings
The AP radiograph displayed an area of increased bone density (sclerosis) within the cortical margins of the distal left femur in the diaphyseal-metaphyseal region, as well as an irregular trabecular pattern and translucent areas surrounded by the sclerotic serpiginous border of healing bone with elevation of the periosteum (Figure 1).1
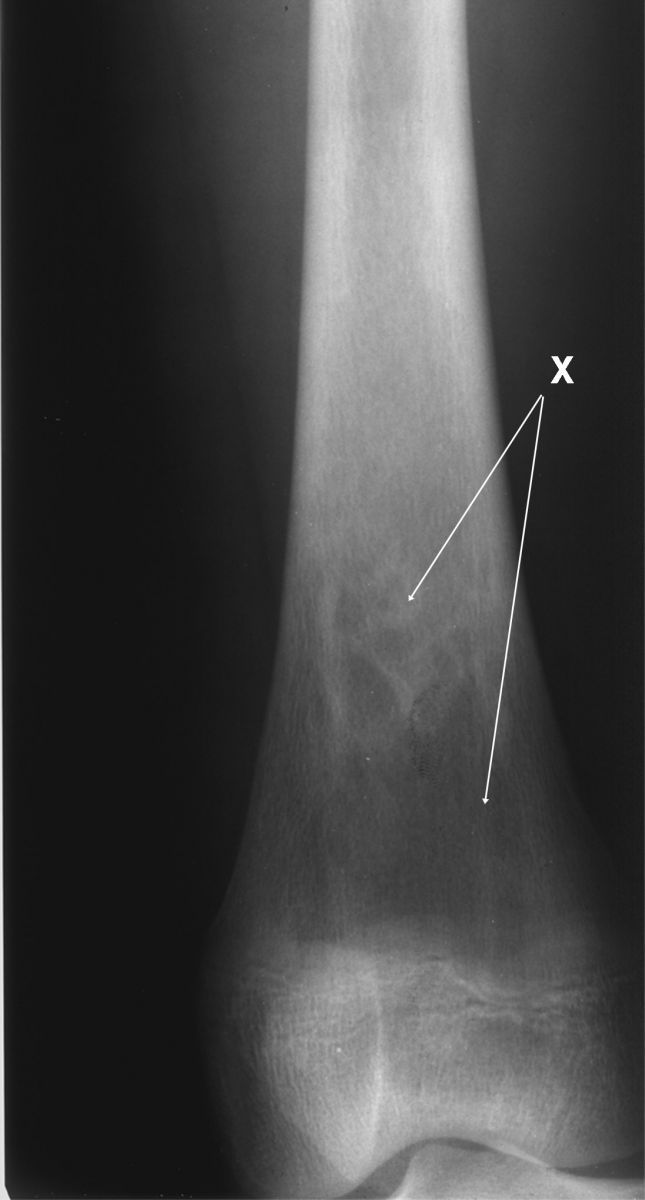
This cone-down radiograph displays periosteal elevation on the lateral surface of the femur (not labeled) and sclerotic serpiginous densities (X) marginated by lucencies in the diaphyselal-metaphyseal region of the left femur.
Figure 1
The AP radiograph was then enlarged over the region of the elevated periosteum displaying fascial plane expansion of inflammation/hemorrhage (Figure 2). The enlarged image caused a high-density artifact medial to the elevated periosteum.
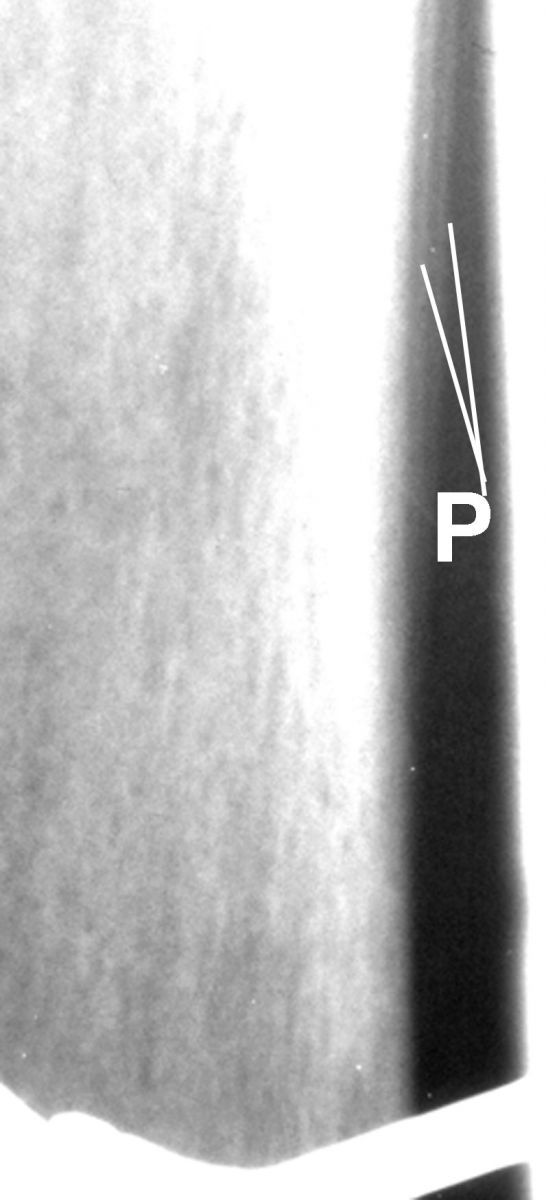
This enlarged image of Figure 1 displays the elevated periosteum (P) reflecting fascial plane expansion of inflammation/hemorrhage. Observe the high dense artifact (not labeled) medial to the elevated periosteum secondary to enlarging the image.
Figure 2
Pathological Diagnosis
A percutaneous biopsy of the distal anterior left femur was performed and demonstrated findings consistent with Gaucher’s cells and bone infarction with no evidence of malignancy.
The boy was tested and declared a carrier of both Gaucher’s disease and sickle cell anemia. He was discharged to return for management and treatment of his described findings. However, he was lost to follow-up.
Further Radiographic Findings
The patient returned 28 years later for additional imaging. He indicated that he was on continuous artificial enzyme treatment for Gauchers’ disease. His AP chest radiograph displayed anterior rotated clavicles over the posterior 3rd intercostal spaces, which reflected mild rounding of the shoulders and normal cardiomediastinal structures, lungs, and osseous anatomy (Figure 3). A lateral radiograph of the cervical spine displayed the normal clavicle, mandible, trachea, and the cervical vertebrae (Figure 4).
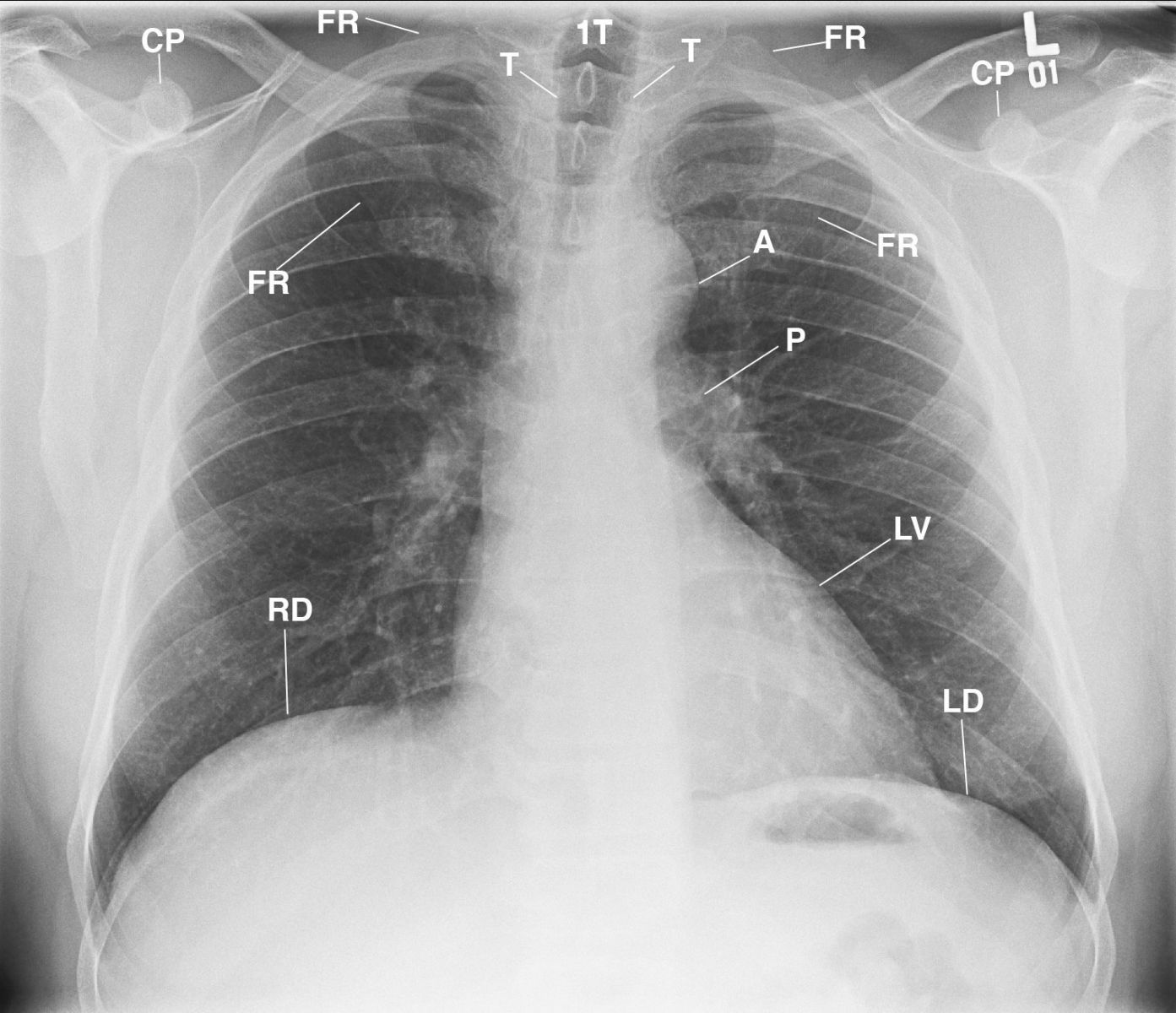
This AP chest radiograph displays the anterior rotated clavicles over the 4th intercostal spaces reflecting mild rounding of the shoulders; normal osseous, cardiomediastinal structures and lungs; and normal air in the stomach (not labeled) reflecting non-enlargement of the spleen. A= aorta; CP= coracoid process; FR= first rib; LV= left ventricle; P= pulmonary artery; RD= right hemidiaphragm; LD= left hemidiaphragm; T= trachea; 1T = first thoracic vertebra.
Figure 3
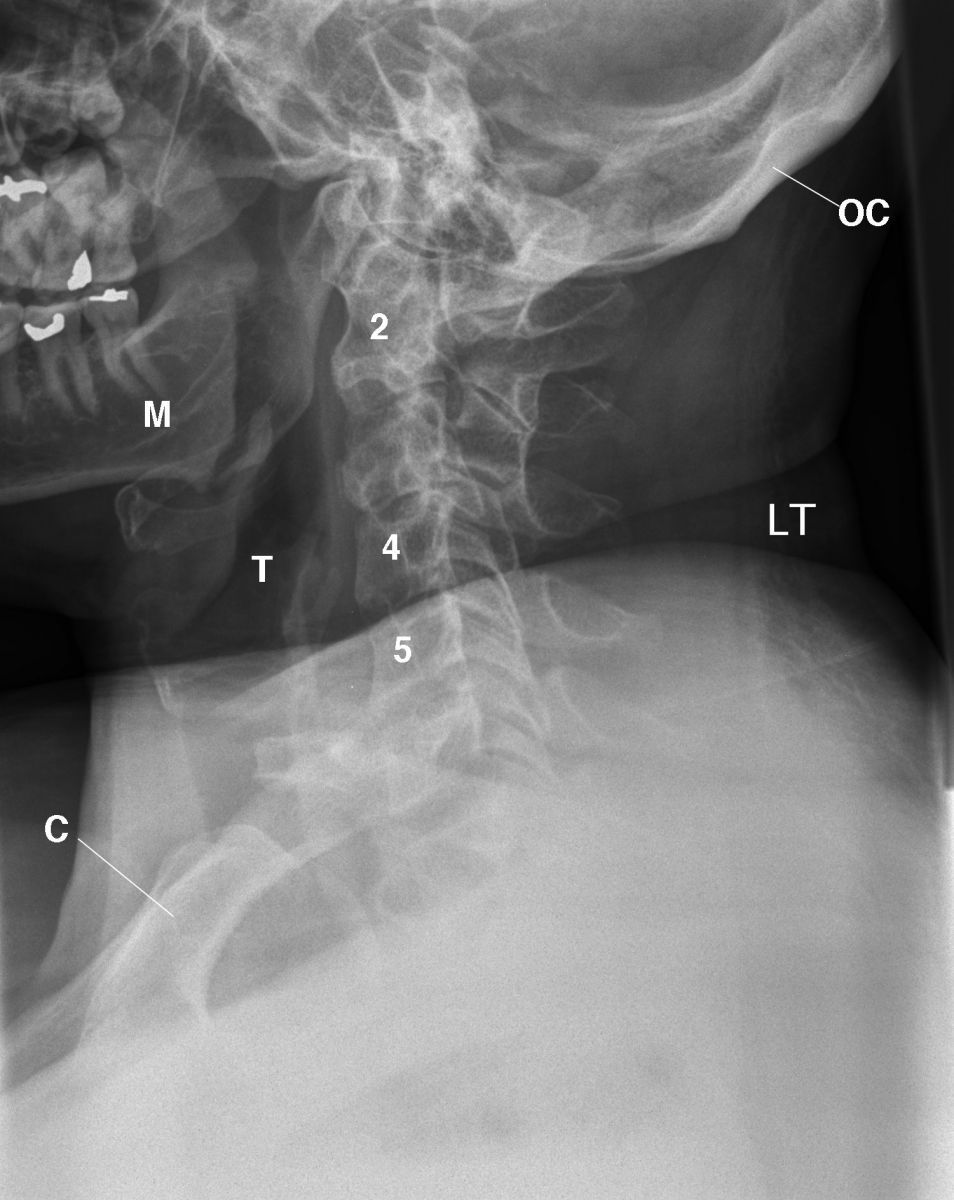
Figure 4 This lateral radiograph of the cervical spine displays the normal clavicle (C), mandible (M), left (LT), trachea (T), cervical spine vertebrae (2, 4, 5), occipital bone (OC), normal articular facets (not labelled), and no osseous abnormalities.
Magnetic resonance imaging of the abdomen, pelvis, and lower extremities was obtained without contrast. The acquired T1-weighted images displayed normal thoracolumbar vertebrae, liver, descending aorta, and spleen (Figure 5). An AP radiograph of the left hip displayed the normal trabecular pattern of the left hip joint and the proximal femur (Figure 6), while an enlarged AP radiograph of the distal left femur displayed dense margins of periostitis and sclerosis in the bone marrow (Figure 7).
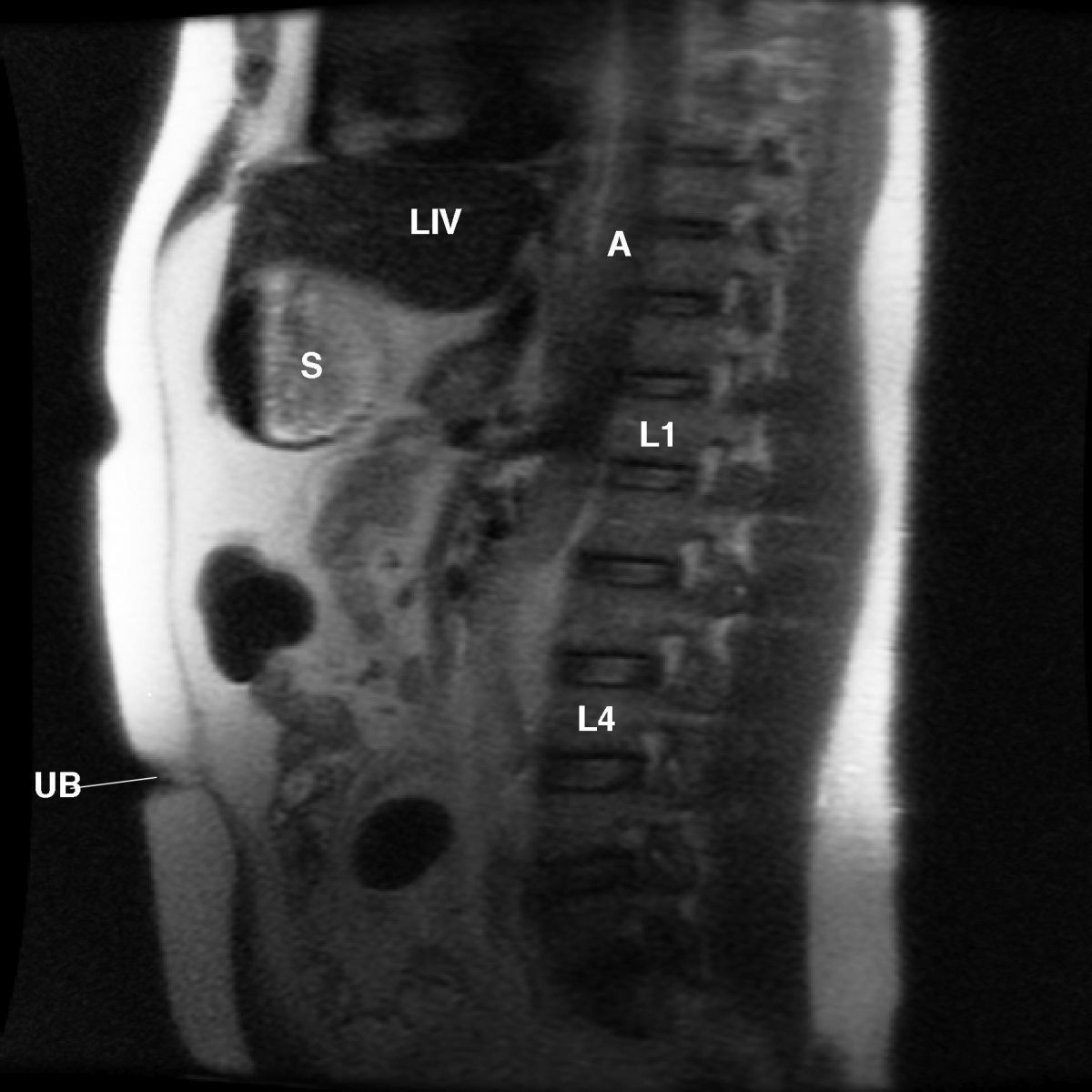
This sagittal MRI radiograph displays the normal thoracic, (not labeled) and lumbar vertebrae (L1, L4). Fascial plane of the rectus abdominus muscle is not labeled. Liv= liver; A= descending aorta; UB= umbilicus; S= stomach.
Figure 5
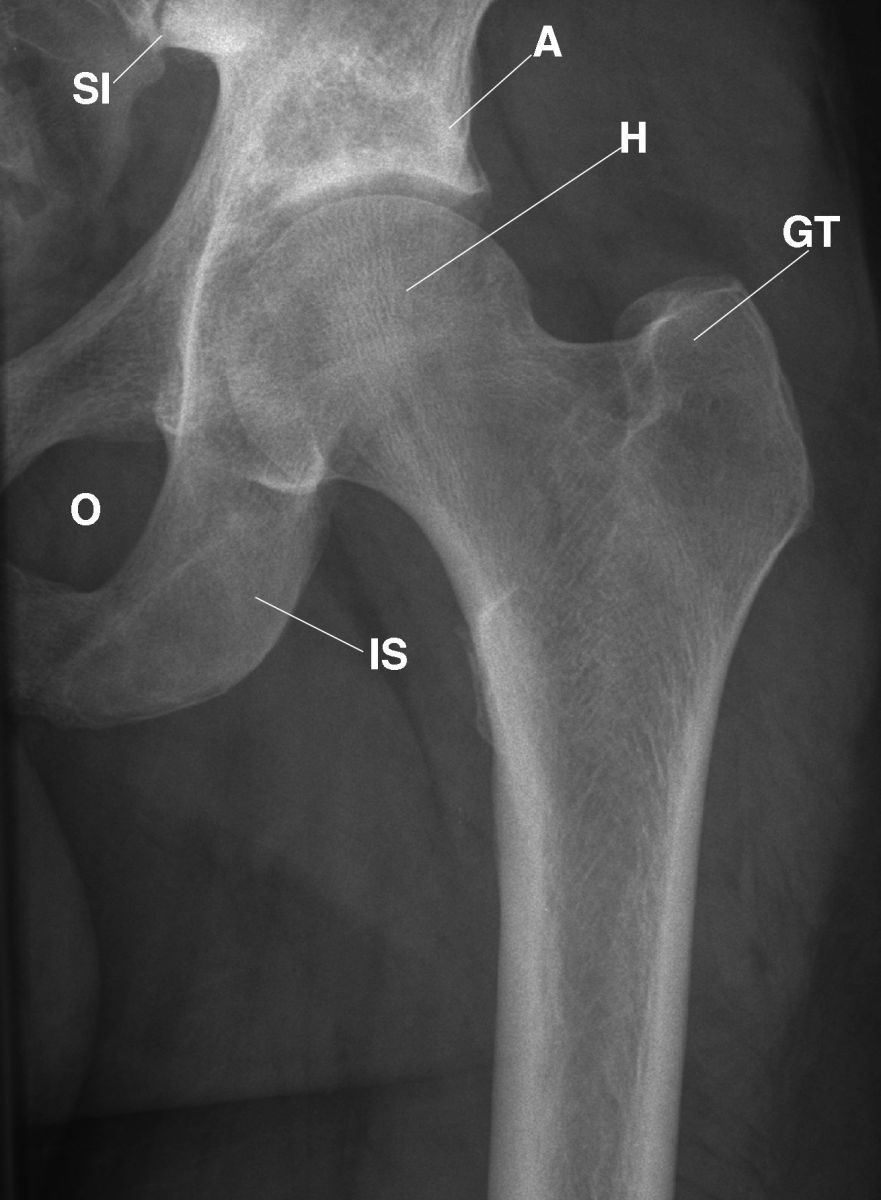
This AP radiograph of the left hip displays the normal appearance of the left hip joint, ischium (IS), acetabulum (A), head of the femur (H), greater trochanter (GT), irregular margin of the lesser trochanter (not labeled), and normal trabecular pattern of the proximal femur, ischium, and pubic bones (not labeled). The adjacent muscles are within normal limits (not labeled).
Figure 6
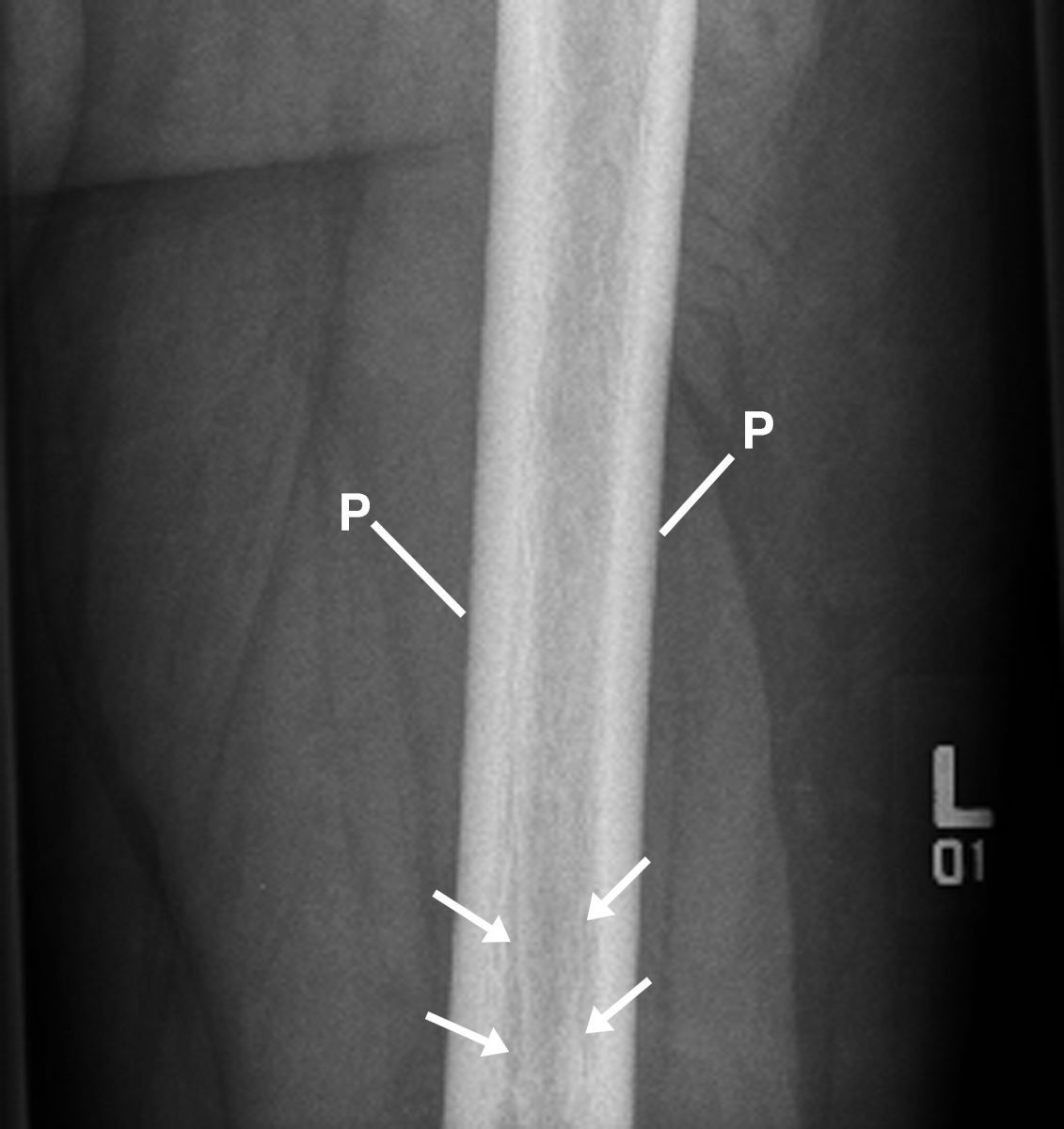
This enlarged AP radiograph displays the dense margin of periostitis (P) and sclerosis in marrow margins within the distal left femur (4 arrows).
Figure 7
An anterior radiograph of the left tibia, fibula, and the talus of the left ankle displayed thickening of the periosteum over the left fibula and thickened cortex of the left tibia (Figure 8). Bilateral T1-weighted coronal images of the femurs displayed high proton-dense fat within the marrow of the femurs and low proton-dense sclerosis (infarction) in the distal diaphyseal-metaphyseal regions of the femurs (Figure 9).

This anterior radiograph displays the left tibia, fibula, and the talus of the left ankle. Observe the thickened periosteum (P) cortical margin of the left fibula (F) and the irregular soft tissues from wearing tight, high boots (E) and the thickened cortex of the left tibia (T)
Figure 8
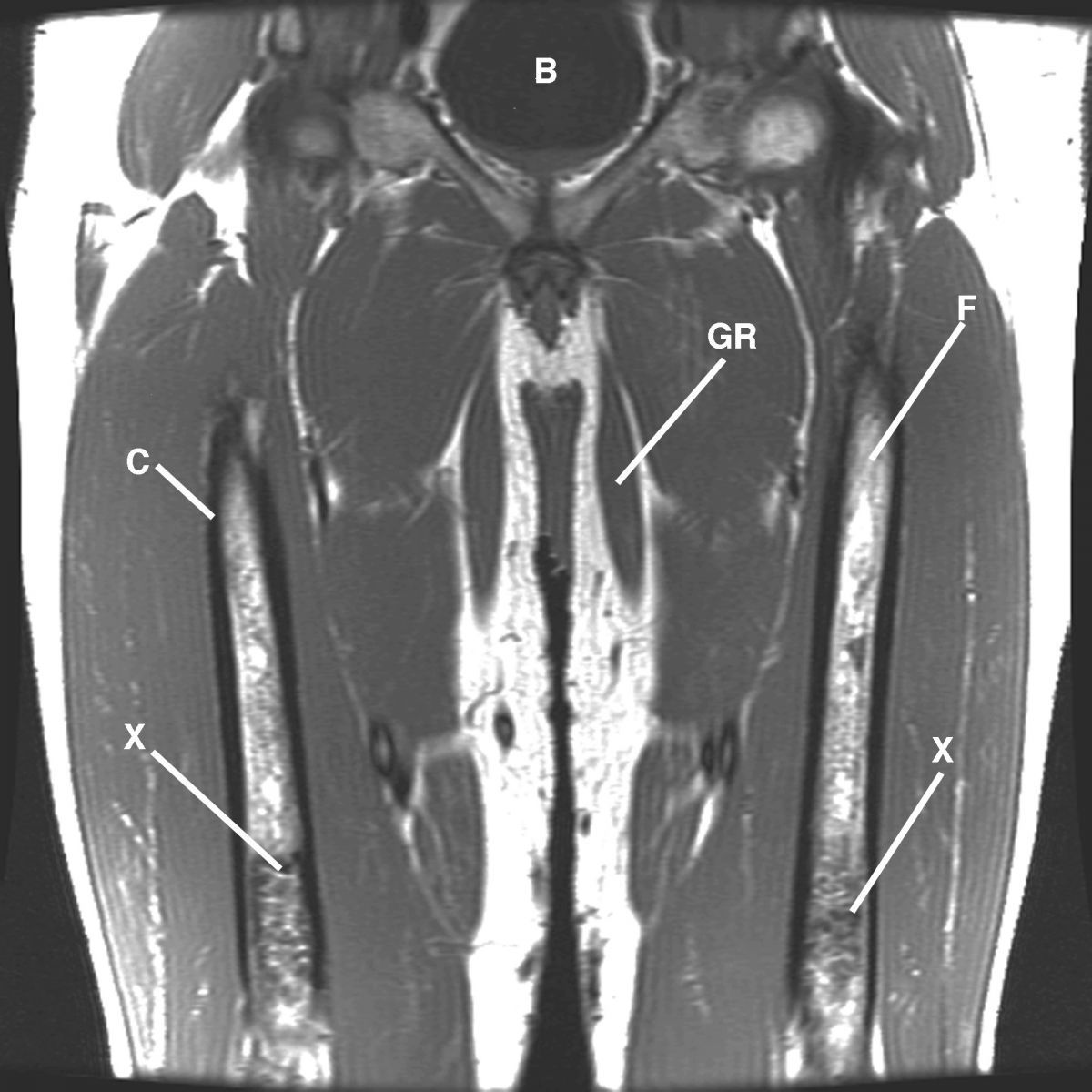
This bilateral T1-weighted coronal image displays the femurs. Observe the high proton-density fat (not labeled) within the femurs (F) and low proton-density sclerosis (infarction) (X) in the distal diaphyseal-metaphyseal regions of the femurs. B= bladder; C= cortex; GR= gracilis muscle.
Figure 9
Differential Diagnosis
Clinical considerations in the differential diagnosis of radiographic findings in Figures 1 and 2 incorporated a wealth of conditions, including avascular necrosis, Caisson’s disease, sickle cell anemia (HbSC and HbSS), thalessemia, Gaucher’s disease, histiocytosis X, osteomyelitis, corticosteriods, thromboembolism, X-irradiation, Fabry disease, Laennec’s cirrhosis, Cushing syndrome, fractures, dislocations, osteochondroses, Legg—Calvé–Perthes disease, Osgood–Schlatter disease, slipped femoral epiphysis, and diseases of the arterial wall, such as systemic lupus erythematosis (SLE), Boeck’s sarcoid, rheumatoid arthritis, and arteriosclerosis.
Discussion
The patient’s history indicated that he is a hereditary carrier of sickle cell anemia and Gaucher’s disease. The pathologic diagnosis indicated that he had bone infarction, which is common to both conditions. Infarction of the spleen also occurs in sickle cell anemia, whereas the spleen is enlarged in Gauchers’ disease. However, neither infarction nor enlargement of the spleen was demonstrated in the patient.
The patient did not present with any of the clinical findings or pathological changes specific to Gaucher’s disease and sickle cell anemia, with the exception of Gaucher’s cells and bone infarction.
Take-Home Message
Gaucher’s disease is an inherited autosomal recessive deficiency of glucocerebrosidase that causes glucocerebroside to accumulate in the spleen, liver, lungs, bone marrow, and sometimes the brain.2-3 Sickle cell anemia occurs when someone inherits 2 specific abnormal genes that cause red blood cells to change shape. Just as in Gaucher’s disease, the condition requires both parents to be carriers of the inherited gene. The patient’s given pathology documented changes compatible with that of his 2 parents.4-5
At the time of the patient’s return after 28 years, he reminded me that his father was a carrier of Gaucher’s disease and his mother was a carrier of sickle cell anemia. It’s important for physicians and healthcare professionals to know the history of the patient’s presenting complaint and as much family history as possible to arrive at an accurate diagnosis.
References
1. Lodwick GS. (1964). Radiologic Clinics of North America: Vol. 11. Number 2. Symposium on Radiology and the Skeletal System.
2. Collins JD, et al. Percutaneous biopsy following positive bone scans. Radiology. 1979 August;132(2):439-42.
3. Collins JD. A young man with an enlarged spleen and pathologic fractures in the long bones. Family Practice Recertification. 2007 August; 29(8):13-5. http://tosinfo.com/pdf/fpr0807.pdf.
4. Lindstrom RR, Collins JD, Byfield JE. Obtaining viable tumor cells through percutaneous pulmonary needle biopsy. Radiology. 1970 January;94(1):200-3.
5. Kohler A. (1968). Borderlands of the Normal Early Pathologic Changes in Skeletal Roentgenology (3rd ed.). New York: Grune & Stratton.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation. Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.