60-Year-Old Man With Skipped Heartbeat, Shortness of Breath and Light-headedness
A 60 year-old man presents with complaints of a skipped heartbeat, shortness of breath and some light-headedness while sitting. When he is active, he has none of these symptoms. He is able to walk, climb stairs and even exercise on his elliptical without symptoms.
A 60 year-old man presents with complaints of a skipped heartbeat, shortness of breath and some light-headedness while sitting. When he is active, he has none of these symptoms. He is able to walk, climb stairs and even exercise on his elliptical without symptoms.
However, when he sits to rest, his symptoms return. His vitals on arrival are taken by the nurse and documented as a heart rate of 55 beats per minute and a blood pressure of 160/90 mmHg.
On exam he is bradycardic with a heart rate in the 30’s. Otherwise his exam was normal. An EKG is performed which is shown below.
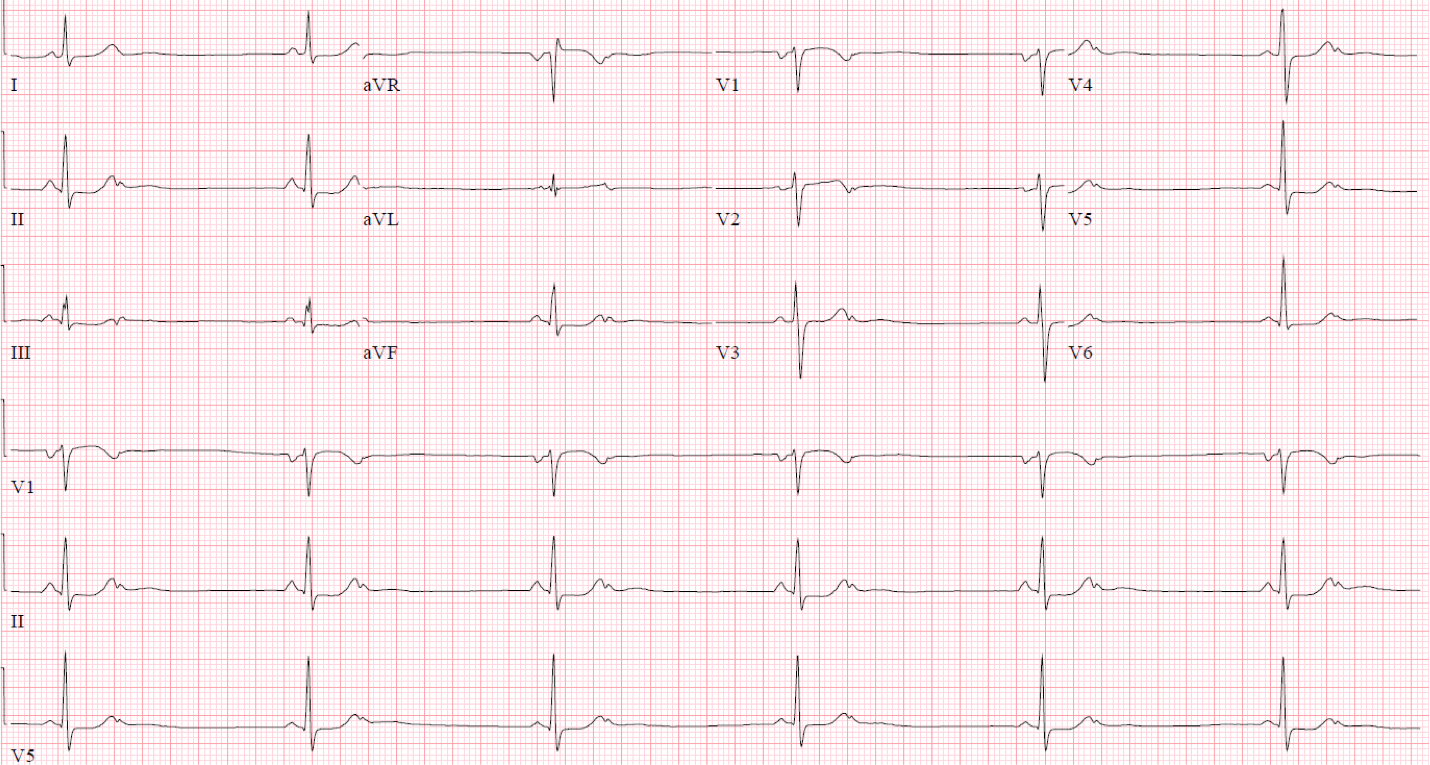
(EKG Rounds 4.1)
Figure 1: Sinus bradycardia with frequent non-conducted premature atrial contractions in an atrial bigeminy pattern.
The ventricular rate is bradycardic and approximately 36 beats per minute. Before each narrow QRS is a P wave with a stable P-R interval. The P waves associated with the narrow QRS complexes are upright in II, III and aVF suggesting that the rhythm originates in the sinoatrial (SA) node.
Looking at the rhythm strips at the bottom of the EKG, the T wave is abnormal with a notched appearance. The notches in the T waves are non-conducted premature atrial contractions, or atrial premature beats (APBs) in a pattern of atrial bigeminy, alternating with normal sinus beats that conduct through the atrioventricular (AV) node.
The 2:1 nature of the block may persuade the reader to think about second degree AV block, but second degree AV blocks have a steady P-P interval and the P waves associated with the APBs present early.
APBs are differentiated from sinus beats by their contour and timing. Because the APB originates in a site other than the SA node, the contour is frequently different morphologically from the P wave associated with sinus rhythm. For instance, if the ectopic focus is close to the AV node, the APB may be down-going in the inferior leads. The easiest way to identify an APB is when the timing of P waves comes in earlier than expected. Lastly, the P-R interval of the APB is often different than the P-R interval associated with the sinoatrial focus.
If the AV node is still refractory from the prior sinus beat, it may not be able to react to the APB resulting in a dropped beat, or a non-conducted APB.
Generally APBs are thought to be benign. However, they can propagate sustained arrhythmias, or be very symptomatic, as they appear to be in this patient.
As an experiment at the bedside, the patient was told to pump his arms and legs and a repeat EKG was performed and is shown below.
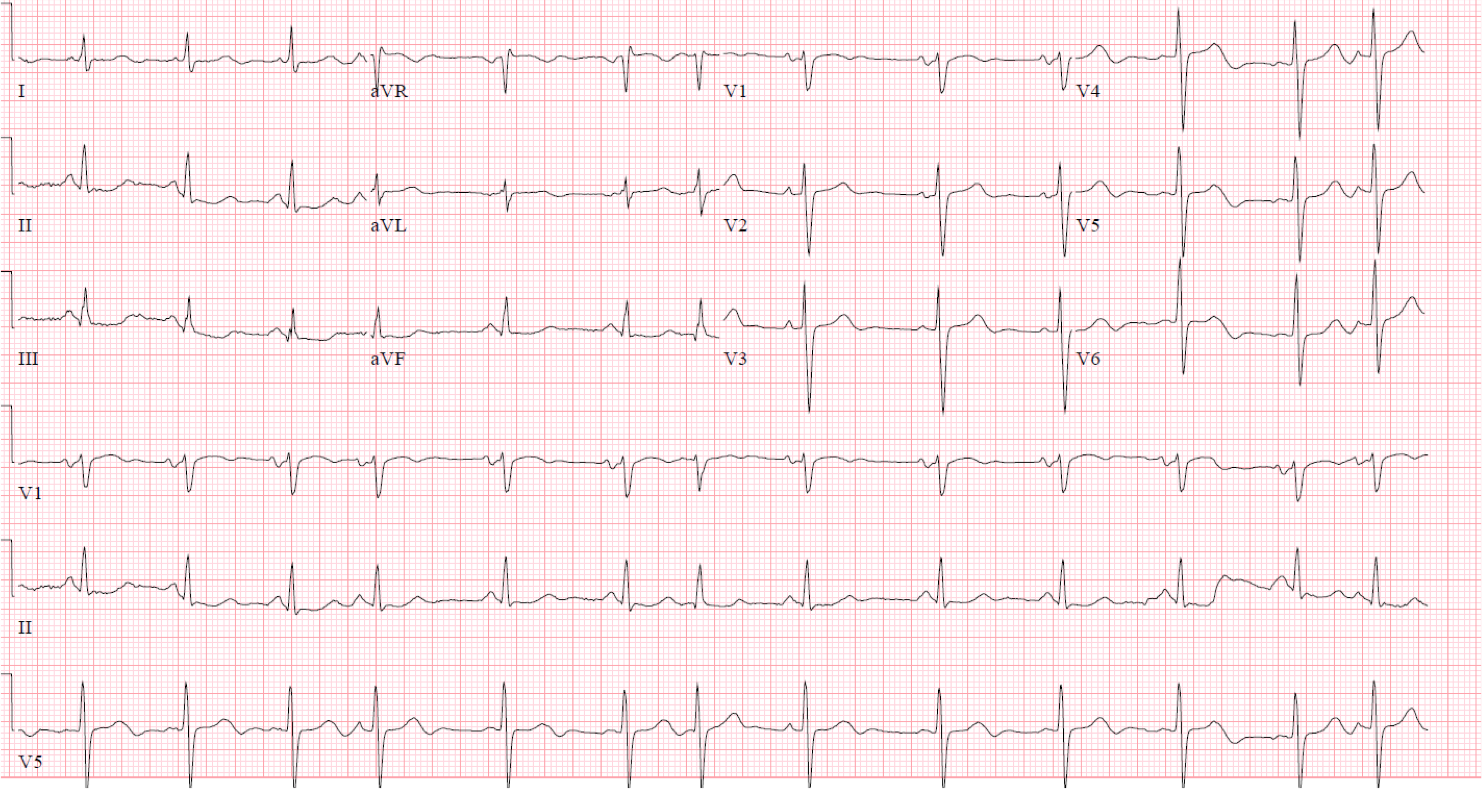
(EKG Rounds 4.2)
Figure 2: Normal sinus rhythm with frequently conducted premature atrial beats.
In the second EKG with exertion, the heart rate has increased to above 70 beats per minute. The APBs remain (beats 4, 7 and 13), but in contrast to the first, ECG, they are now conducted. As he exerts himself, his sympathetic tone decreases the refractoriness of the AV node and the APBs are able to conduct through to the ventricles thereby eliminating the dropped beats.
This explains why he felt improved with exertion. However, he continued to have symptoms at rest. A trial of beta-blockers was attempted to decrease the automaticity of the APBs, but that resulted in further slowing of his sinus rate without decreasing the APB burden. He was referred to an electrophysiologist and ablation was recommended as a curative measure. The patient was initially hesitant to undertake an invasive procedure and preferred a trial of flecainide.
Flecainide is a class IC antiarrhythmic that works by blocking sodium channels reduces the excitability in the heart and can be useful for tachyarrhythmias. However, adverse side effects are possible and antiarrhythmics should be used carefully. Flecainide should never be used in patients with heart failure or ischemic heart disease and care must be taken to watch for cardiac toxicity leading to fatal ventricular arrhythmias.
Although the patient’s symptoms were reduced on flecainide with less APB’s, he still felt his worst whenever he was at rest. Due to the failure of the flecainide to control his symptoms, he proceeded to APB ablation with subsequent successful termination of the APB focus and resolution of his symptoms.
1. Dobrzynski H, Anderson RH, Atkinson A, et al. Structure, function and clinical relevance of the cardiac conduction system, including the atrioventricular ring and outflow tract tissues. Pharmacol Ther. 139(2):260—288.
2. Thaler M. The only EKG book you will ever need. 7th. Lippincott 2012.