ACR Proposes Recommendations for Glucocorticoid-Induced Osteoporosis
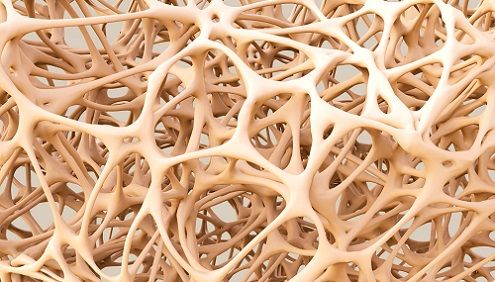
Used for treatment of inflammation in rheumatic diseases, glucocorticoids are known to cause osteoporosis. The American College of Rheumatology has put forth new recommendations to hopefully decrease the frequency of bone fractures.
At the 2016 American College of Rheumatology Annual Meeting in Washington, D.C., principal investigator Lenore Buckley detailed draft recommendations for an update to the organization’s 2010 guidelines for the prevention and treatment of glucocorticoid-induced osteoporosis.
Used for treatment of inflammation in rheumatic diseases, glucocorticoids are known to have negative effects on bone mass, leading to osteoporosis. About 1% of the population uses this class of steroid, according to Buckley, and the most common adverse effect is fracture, whether spinal or of the hip. “We know that the risk is dose-related,” she says, “So the more you take, the more the risk, and the longer you take it, the greater the risk.”
In order to hone their work, they first pondered who they were making recommendations to and what they were making them about. Glucocorticoid treatment often varies over time, with patients going on and off and changing doses frequently, so they wanted their new guidelines to be dynamic as well.
The first set of suggestions involved risk assessment, taking into account not just glucocorticoid use but also lower mass based on age, gender, and race demographics. They suggested using FRAX as a way of calculating 10-year facture risk, though it only contains data for men and women over the age of 40. Glucocorticoid use is an input factor in FRAX, and the draft recommends ways of interpreting results relative to dosage.
For people under the age of 40, there is no fracture risk calculator. The committee deemed people under the age of 40 who had already had one glucocorticoid-related fracture were deemed “high risk.”
A new recommendation not featured in the 2010 guidelines was the definition of a “moderate risk” group. Men and women with low bone mass or who had undergone greater than 10% bone loss over the course of a year of continued glucocorticoid treatment. People with none of those risk factors were put in a “low risk” group.
The panel suggested an initial assessment of osteoporosis risk before glucocorticoid treatment in addition to bone mass assessments every two or three years.
For the treatment of glucocorticoid-induced osteoporosis, the group made suggestions of medication based on risk factor. Moderate-to-high risk people, whether under or over the age of 40, were recommended first and foremost the use of oral bisphosphonates, followed by IV bisphosphonates, teraparatide, and lastly, denosumab. Calcium and vitamin D were recommended for all risk groups.
Speaking to MD Magazine about the rationale behind the ranking, Buckley said efficacy, convenience and cost were the major factors. “The IVs were second because there’s some suggestion of greater risk with them, not a lot greater but slightly, and more cost. Teraparatide, since it’s an injectable you have to give yourself every day, it has some patient inconvenience and some cost reasons. Denosumab is very expensive.”
“There isn’t really very good data, though we all have our beliefs, that any one is greater for fracture rates than the others,” she explained, “There is some data on how bone density might change by class, but patients care about fractures. There wasn’t any evidence that any one was more effective than any other, but cost was an issue, patient convenience, and side effects.”
The committee also made recommendations for special populations, including women with childbearing potential. Oral bisphosphonates were still recommended first for them, but teraparatide was considered the second-best option due to the fact that it works quickly. IV bisphosphonates and denosumab were considered to carry fetal toxicity risk in the event of an unplanned pregnancy.
Another special population were people with organ transplants, whom they recommended follow the general age-related guidelines with exceptions in the case of those without good kidney function or in whom the kidney had been the transplanted organ, for whom they advised against denosumab.
Children were the third special population. Calcium and vitamin D were endorsed, and oral and then IV bisphosphonates were the top recommendations.
The final risk group were those on very high doses of glucocorticoids, exceeding 5 grams per year, who are seen as at a very high risk. Oral bisphosphonates were again the primary recommendation.
General recommendations included still monitoring risk of fracture following cessation of glucocorticoid treatment and attempting other treatments for those who failed treatment on oral bisphosphonates.
The draft recommendations will soon face peer review before an intended finalization and publication in 2017.
Related Coverage:
Study Finds Abaloparatide Can Stimulate Bone Formation in Osteoporosis
Continuing Treatment in Postmenopausal Women with Osteoporosis
Anti-TNF Treatments for Ankylosing Spondylitis Decrease Need for Hip Replacement