Aortic Stiffness, Blood Pressure Progression, and Incident Hypertension
Karla K. Quevedo, MD
Kaess BM, Rong J, Larson MG, et al. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA. 2012;308:875-881.
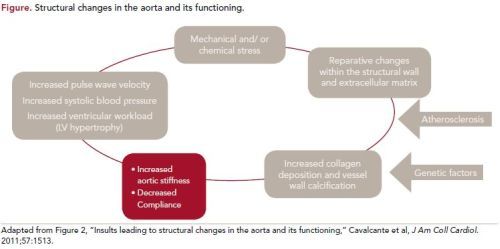
Stiffening of the aortic wall is a major risk factor for cardiovascular morbidity and mortality. The association between vascular stiffness (Figure) and hypertension is likely bidirectional.Nevertheless, the temporal relationship remains incompletely elucidated. The study by Kaess et al evaluates vascular stiffness, central hemodynamics, peripheral blood pressure, and incident hypertension in the Framingham Heart Study Offspring cohort.
Study Details
This longitudinal community-based cohort study is based on the 2 latest examination cycles (cycle 7: 1998-2001; cycle 8: 2005-2008) of the Framingham Offspring study. Participants had follow-up examinations at the Heart Study clinic every 4 to 6 years, which included standardized questionnaires, physical examination [blood pressure measured using standardized protocol, pulse pressure and mean arterial pressure (MAP)], and assessment of standard cardiovascular risk factors. Hypertension was defined as a systolic blood pressure (SBP) of ≥140 mm Hg, diastolic blood pressure (DBP) of ≥90 mm Hg, or the use of antihypertensive medication. Arterial stiffness (AS) and pressure pulsatility derived from arterial tonometry were evaluated using 3 measurements: carotid-femoral pulse wave velocity (CFPWV), central forward pressure wave amplitude (FWA), and augmentation index. Brachial artery flow velocity and flow-mediated dilation (FMD) were also measured.
The primary outcomes were continuous SBP, DBP, MAP, and pulse pressure during examination cycle 8 as well as incident hypertension during examination cycle 7. The secondary outcomes were CFPWV, FWA, and augmentation index. Incident hypertension correlation was assessed in a 3-stage design using a multivariate logistic regression model. In the first phase researchers investigated clinical (age, sex, BMI, height, heart rate, diabetes, lipid-lowering treatment, prevalent cardiovascular disease, current smoking, and time between cycles 7 and 8) and biochemical variables (total cholesterol, high-density lipoprotein cholesterol, triglycerides, and fasting glucose) during examination cycle 7 that were associated with at least 1 of the assessed continuous outcomes in a multivariate model.
In a second stage, researchers identified BP and tonometry measures collected in cycle 7 that were associated with the continuous outcome in multivariate models. In a third stage, the study investigated whether brachial flow or FMD further improved the regression models. Of the 3539 participants from cycle 7, 1263 (36%) were excluded due to insufficient data. Of the 2276 participants who met study criteria during examination cycle 7, 1759 (77%) continued during examination cycle 8 and were the primary sample for the study. For the analysis of incident hypertension, 711 participants (40%) were excluded due to prevalent hypertension during cycle 7 examination, resulting in 1048 cases, of whom 338 (33%) cases were diagnosed with incident hypertension during cycle 8 examination. In the regression model, higher FWA and higher CFPWV during examination cycle 7 were associated with higher SBP during examination cycle 8. Lower SBP and CFPWV during examination cycle 7 were associated with higher DBP during examination cycle 8.
Also, lower baseline and higher hyperemic forearm blood flow during examination cycle 7 were associated with higher DBP during examination cycle 8. Higher FWA, CFPWV, and augmentation index and lower MAP during examination cycle 7 were associated with higher pulse pressure during examination cycle 8.
It was observed that SBP, DBP, FWA, augmentation index, and CFPWV considered together in a single multivariate model were associated with incident hypertension
during examination cycle 8. Higher baseline brachial arterial flow and lower FMD in cycle 7 examination were associated with incident hypertension during examination cycle 8. A higher CFPWV, lower DBP, and higher pulse pressure in cycle 7 examinations were associated with a higher FWA measure during examination cycle 8. The primary outcome of the study was to evaluate the longitudinal relationship among aortic stiffness, central hemodynamic, microvascular properties, and peripheral BP. The study demonstrated prospectively that 3 important tonometry measures—CFPWC, FWA, and augmentation index—were related to future SBP, pulse pressure, and incident hypertension. BP traits were associated with future FWA and augmentation index, but not with future CFPWV. The study also demonstrated that higher AS
was a predictor of incident hypertension, whereas higher baseline BP was not a predictor of increased AS. Baseline BP was not independently associated with future CFPWV when analysis was adjusted for initial CFPWV and cardiovascular risk factors. In addition, brachial artery measures of microvascular resistance and endothelial function were jointly associated with incident hypertension after taking into account BP and tonometry variables.
References
1. Mattace-Raso FU, Van der Cammen TJ, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113:657-663.
2. Laurent S, Boutouyrie P, Asmar R. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:
1236-1241.
3. Laurent S, Katsahian S, Fassot C, et al. Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke. 2003;34:1203-1206.
4. Lehmann ED, Parker JR, Hopkins KD, Taylor RG, Gosling MG. Validation and reproducibility of pressure-corrected aortic distensibility measurements using pulse-wave
velocity Doppler ultrasound. J Biomed Eng. 1993;15:221-228.
5. Asmar R, Benetos A, Topouchian J, et al. Assessment of arterial distensibility by automatic pulse wave velocity measurement. Validation and clinical application studies. Hypertension. 1995;26:485-490.
6. Najjar SS, Scuteri A, Shetty V, et al. Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of Aging. J Am Coll Cardiol. 2008; 51:1377-1383.
7. Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice. Eur J Cardiovasc Prev Rehabil. 2007;14(suppl 2):E1-E40.
8. Mancia G, De Backer G, Dominiczak A, et al. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC). J Hypertens. 2007;25:1751-1762.
9 Dernellis J, Panaretou M. Aortic stiffness is an independent predictor of progression to hypertension in nonhypertensive subjects. Hypertension. 2005;45:426-431.
10. Najjar SS, Scuteri A, Shetty V, et al. Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of Aging. J Am Coll Cardiol. 2008; 51:1377-1383.
11. Asmar R. Effect of antihypertensive agents on arterial stiffness as evaluated by pulse wave velocity: clinical implications. Am J Cardiovasc Drugs. 2001;1:387-397.
Benetos A, Vasmant D, Thiery P, Safar M. Effects of ramipril on arterial hemodynamic. J Cardiovasc Pharmacol. 1991;18(suppl 2):S153-S156.
12. Heesen WF, Beltman FW, Smit AJ, et al. Reversal of pathophysiologic changes with long-term lisinopril treatment in isolated systolic hypertension. J Cardiovasc Pharmacol. 2001;37:512-521.
13. Ting CT, Chen CH, Chang MS, Yin FC. Short- and long-term effects of antihypertensive drugs on arterial reflections, compliance, and impedance. Hypertension. 1995;26:524- 530.
14. London GM, Safar ME, for the REASON Project Investigators. Mechanisms of selective systolic blood pressure reduction after a lowdose combination of perindopril/indapamide in hypertensive subjects: comparison with atenolol. J Am Coll Cardiol. 2004;43:92-99. 15. Pirro M, Schillaci G, Mannarino MR, et al. Effects of rosuvastatin on 3-nitrotyrosine and aortic stiffness in hypercholesterolemia. Nutr Metab Cardiovasc Dis. 2007;17:436- 441.
16. Kass DA, Shapiro EP, Kawaguchi M, et al. Improved arterial compliance by a novel advanced glycation end-product crosslink breaker. Circulation. 2001;104:1464-1470.
17. Kakiyama T, Matsuda M, Koseki S. Effect of physical activity on the distensibility of the aortic wall in healthy males. Angiology. 1998;49:749-757.
18. Phillips CL, Yee B, Yang Q, et al. Effects of continuous positive airway pressure treatment and withdrawal in patients with obstructive sleep apnea on arterial stiffness and central BP. Chest. 2008;134:94-100.
Commentary
A Potential Marker of Increased LV Load Preceding Systemic Hypertension
AS is one of the earliest detectable signs of adverse structural and functional changes within the blood vessel wall and has been shown to be an independent predictor of coronary heart disease and stroke in healthy subjects and an independent predictor of mortality in the general population.1 In general, increased AS has been associated with increased morbidity and both all-cause and cardiovascular mortality in hypertensive patients. 2,3
The use of different imaging modalities for assessment of vascular elasticity and quantification of luminal and vessel wall parameters allow for a comprehensive view of the vascular system. Pulse wave velocity (PWV) is the most validated method to noninvasively quantify AS and is considered the gold standard index of AS given its simplicity, accuracy, reproducibility, and strong predictor of adverse outcomes.4,5 PWV is the distance traveled by the wave divided by the time for the wave to travel that distance at 2 sites along a vascular segment. PWV is inversely related to vascular compliance; hence, a stiffer vessel conducts the pulse wave faster than a more distensible and compliant vessel. CFPWV can be used as an estimate of arterial PWV through the entire aorta and is obtained using applanation tonometry and oscillometric method. CFPWV is considered a predictor of future changes in SBP and future development of hypertension in healthy individuals, and can have a role identifying patients at risk of development of hypertension.6 Aortic PWV has been recommended by the 2007 European guidelines for the management of hypertension and guidelines for cardiovascular disease prevention in clinical practice to assess target organ damage.7,8
The Kaess et al study is one of the few to assess the relationship among tonometry measures and BP progression. Dernellis and Panaretou demonstrated that higherproximity aortic stiffness was associated with incident hypertension.9 Najjar et al demonstrated that higher CFPWV was associated with an increase in SBP and incident hypertension.10 In the present study, the findings support the concept that vascular stiffness is a precursor rather than the result of hypertension; therefore, AS can potentially be defined as a marker of increased left ventricular load that might precede the onset of systemic hypertension. AS could be considered a unique entity whose early detection and proper treatment can decrease cardiovascular mortality in the general population and in patients with already established cardiovascular disease.
If AS is a real precursor of hypertension, it is reasonable to target it before hypertension has developed. In fact, many studies have shown that antihypertensive medications could improve AS,11 including ACE inhibitors,12-14 a combination ACE inhibitor-diuretic,15 statins,16 and advanced glycation end-product cross link breakers.17 Nonpharmacologic interventions to reduce AS have also been studied, including increased physical activity18 and continuous positive airway pressure (CPAP) in patients with severe obstructive sleep apnea.19 Further studies are needed to find the best therapeutic approach for AS.
Several limitations of the study should be pointed out. These include a possible underestimation of the relationship among BP progression and tonometry measures because a proportion of cases were receiving antihypertensive treatment during examination cycle 7 or could have received new or higher doses of medications between
cycles. Because FWA was calculated by 2 different methods during cycles 7 and 8, respectively, there could have been a misclassification of FWA during cycle 7, causing a change in FWA. Participants were middle-aged to older adults of European ancestry; thus, findings may not be generalizable to younger individuals or ethnic and racial
minorities.
In conclusion, the Kaess et al study demonstrated that aortic stiffness, central FWA, and wave reflection are jointly associated with future SBP, pulse pressure, and incident hypertension. Initial BP traits were associated with future FWA and augmentation index but not with CFPWV. These findings support the concept that vascular
stiffness is a precursor, and not a result of, high BP. AS has proven to be an important determinant of cardiovascular morbidity and mortality. Its early identification
and treatment could prevent the development of hypertension, which could represent a major preventive strategy. Testing for alterations in arterial function and structure could eventually help refine cardiovascular risk assessment in the intermediate-risk groups and identify candidates for aggressive therapy.
About the Author
Karla K. Quevedo, MD, is a Cardiology Fellow at Texas Tech University Health Sciences Center in El Paso, Texas. Dr Quevedo received her MD at the Universidad San Martin de Porres in Peru. She was chief resident in internal medicine at Guillermo Almenara Hospital in Lima, Peru. Her areas of interest are general cardiology, preventive cardiology, and heart failure and biomarkers.
