Diagnosing Ankylosing Spondylitis
This is a 60-year-old male with a 30-year history of bone pain. He had bilateral hip replacements 2 and 3 years earlier with no complications, but he has continued to have severe back pain.
James D. Collins, MD
History
This is a 60-year-old male with a 30-year history of bone pain. He had bilateral hip replacements 2 and 3 years earlier with no complications, but he has continued to have severe back pain.
Radiographic Findings
The principal sites of involvement are the sacroiliac joints (SI) and the spine. Initial radiographic findings may be a loss of definition of the joint margins, but, erosions may also occur. The iliac borders are affected before the sacral margins. Joint spaces may also be narrowed and some patients progress to fibrosis and bony ankylosis.
Spinal changes consist of arthritis of the apophyseal joints, osteitis of the vertebral bodies, syndesmophyte formation (ossification of the outer lamellae of the annulus fibrosis), disk degeneration, erosions, kyphosis, subluxations, and ankylosis.
The anterior posterior (AP) thoracic spine radiograph (Figure 1) displays squaring of the vertebrae and myelographic contrast enhancement within the spinal canal.

Figure 1. This anterior posterior view of the thoracic spine displays squaring off the vertebrae (small arrows) and myelographic contrast (bar arrows) that is residual from earlier radiographic studies. An ascending calcification of the vertebral ligaments leading to a “bamboo spine” is characteristic of ankylosing spondylitis
The lateral view of the kyphotic thoracic spine (Figure 2) displays disk calcification and calcification of the annulus fibrosis of the intervertebral disk. This process is also referred to as syndesmophyte formation.
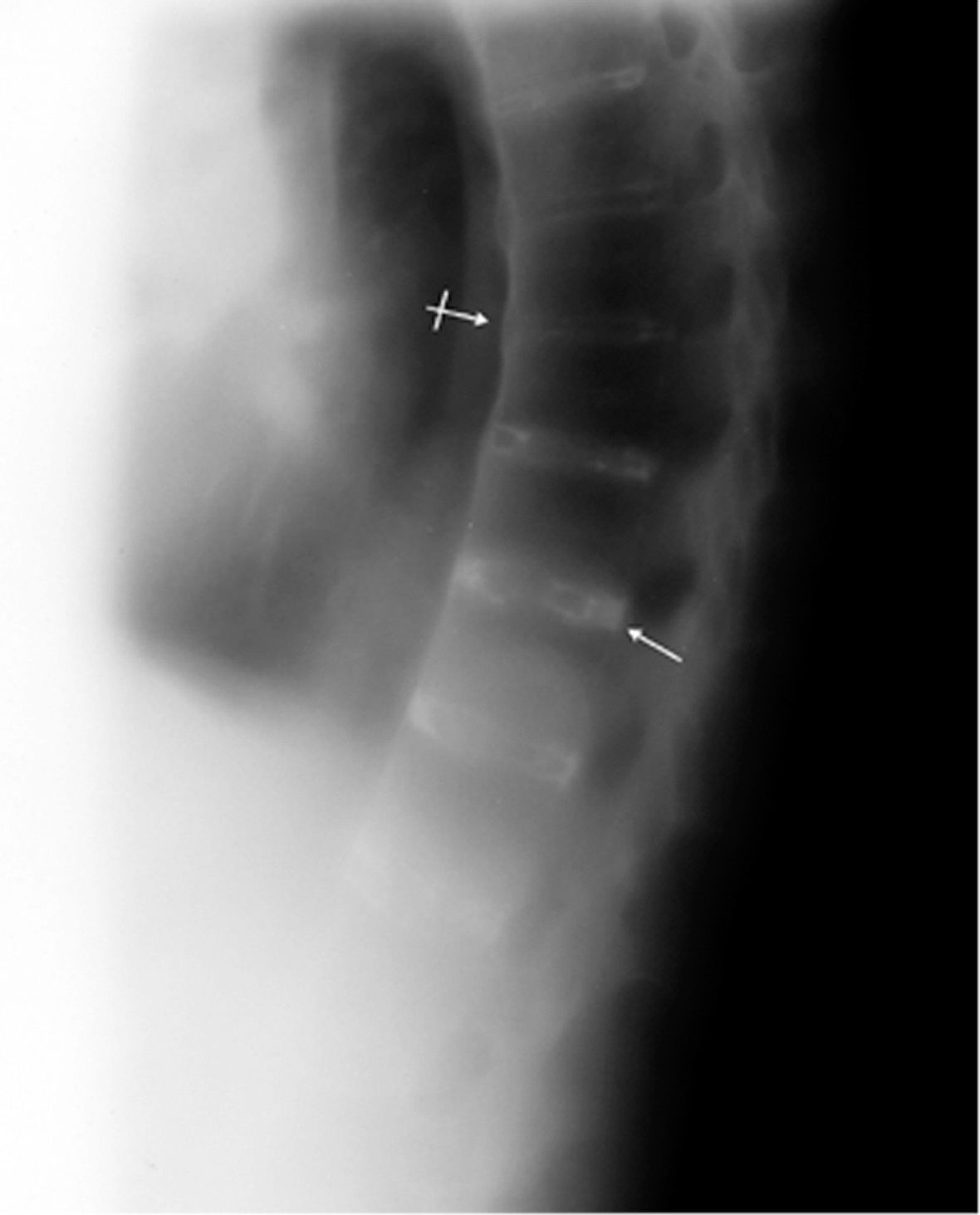
Figure 2. This lateral view of the patient’s kyphotic thoracic spine displays disk calcification (arrow) and calcification of the annulus fibrosis of the intervertebral disk (bar arrow).
The AP pelvic radiograph (Figure 3) displays bony ankylosis of the sacroiliac joints and hip joints.

Figure 3. This anterior posterior view of the pelvis displays ankylosis (fusion) or obliteration of the sacroliac joints (bar arrows) hip joints (arrows).
Diagnosis
This patient’s diagnosis is ankylosing spondylitis, a chronic progressive arthritis that typically involves the sacroiliac and spinal apophyseal joints and the paravertebral soft tissues. Syndesmophyte formation is characteristic of this condition.
Discussion
The onset of this disease is usually insidious. It can include low back pain, sacroiliac or hip pain, or less commonly pain in a sciatic distribution. The age of onset is usually in a patient’s late 20’s or early 30’s and approximately 90% of the patients are men. The sacroiliac joints are almost invariably involved. The hips are involved in about 50% of patients, and the shoulders and knees in 30%.
Ankylosing spondylitis usually starts in the lower lumbar intervertebral joints. Results of synovial fluid analysis in ankylosing spondylitis are similar to those of rheumatoid arthritis. Morphologic features of proliferative chronic synovitis involving the diarthrodial joints are also difficult to distinguish from those of rheumatoid arthritis. Patients with ankylosing spondylitis are negative for rheumatoid factor, however, and they will not have the characteristic subcutaneous nodules of rheumatoid arthritis.
An ascending calcification of the anterior and lateral vertebral ligaments is often displayed in ankylosing spondylitis leading to a “bamboo” or rigid spine. The disease may arrest at any stage or progress to spinal rigidity and kyphosis of the thoracic spine. The cervical spine is involved later in the disease process.
Take-home Message
The diagnosis of ankylosing spondylitis is usually made by a rheumatologist and usually requires X-ray evidence of sacroilitis, or inflammation of the sacroiliac joint.
One of three key findings may be present: low back pain and stiffness for more than 3 months, which improves with exercise, but is not relieved by rest; limited motion of the lumbar spine in both the bending to the side and to the front; limitation of chest expansion relative to normal values corrected for age and sex.
In the early course of the disease, X-ray evidence is required by the above criteria but may not be present. Treatment may begin without the X-ray evidence. A blood test for the presence of the HLA-B27 genetic marker will enhance the diagnosis.
Since inflammation of the vertebral column causes radicular pain, fibrosis and calcification of the ligaments in ankylosing spondylitis, fascial plane landmark anatomy is altered (pathology). Therefore, it’s reasonable to believe that the vertebral venous plexus (Batson’s plexus) of the vertebral column would be compromised. Any decrease in venous return increases intracranial, intrathoracic and intraabdominal pressure. Triggers patient complaints.2
References
1. Taurog JD, Lipsky PE. Ankylosing spondylitis, reactive arthritis, and undifferentiated spondyloarthropathy. In Fauci AS, Braunwald E. Isselbacher KJ, et al, eds. Harrison’s Principles of Internal Medicine. 14th ed. New York, NY: McGraw Hill; 1998:1904-1909.
2. Woodburne RT, Burkel WE. Essentials of Human Anatomy. 8th ed. New York, NY: Oxford University Press; 1988;18-216.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation.
Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.