News
Article
Experts' Perspectives: Top Story in Heart Failure for 2023
Author(s):
A group of 9 experts in heart failure, ranging from leading trialists to early career clinicians, provide perspective on what they see as the biggest news in heart failure from 2023.
Few fields can lay claim to the level of advancements and breakthroughs as heart failure in the last decade. Not only has the field been the beneficiary of novel agents ascending into guideline-directed medical therapy, but it has also witnessed revelations surrounding the overlap of cardiometabolic disease give birth to a new concept: cardiovascular-kidney-metabolic syndrome, which the American Heart Association recently recognized in a scientific statement.
With trials in heart failure headlining major cardiology meetings year after year for the last half-decade, many could see 2023 as a “quieter” year for the field. However, the number of notable advances occurring within heart failure for 2023 might still be considered historic for many other disease states.
With the Heart Failure Society of America 2023 Annual Scientific Meeting serving as the final heart failure-specific meeting for the year, the editorial team of HCPLive Cardiology polled their interview guests from HFSA 2023 on what they believed was the headlining story in heart failure from the past year to capture the sentiment of key opinion leaders within heart failure.
Found below are the responses of 9 guests, from leading trialists to early career clinicians, who took part in interviews during HCPLive Cardiology's on-site coverage of HFSA 2023.
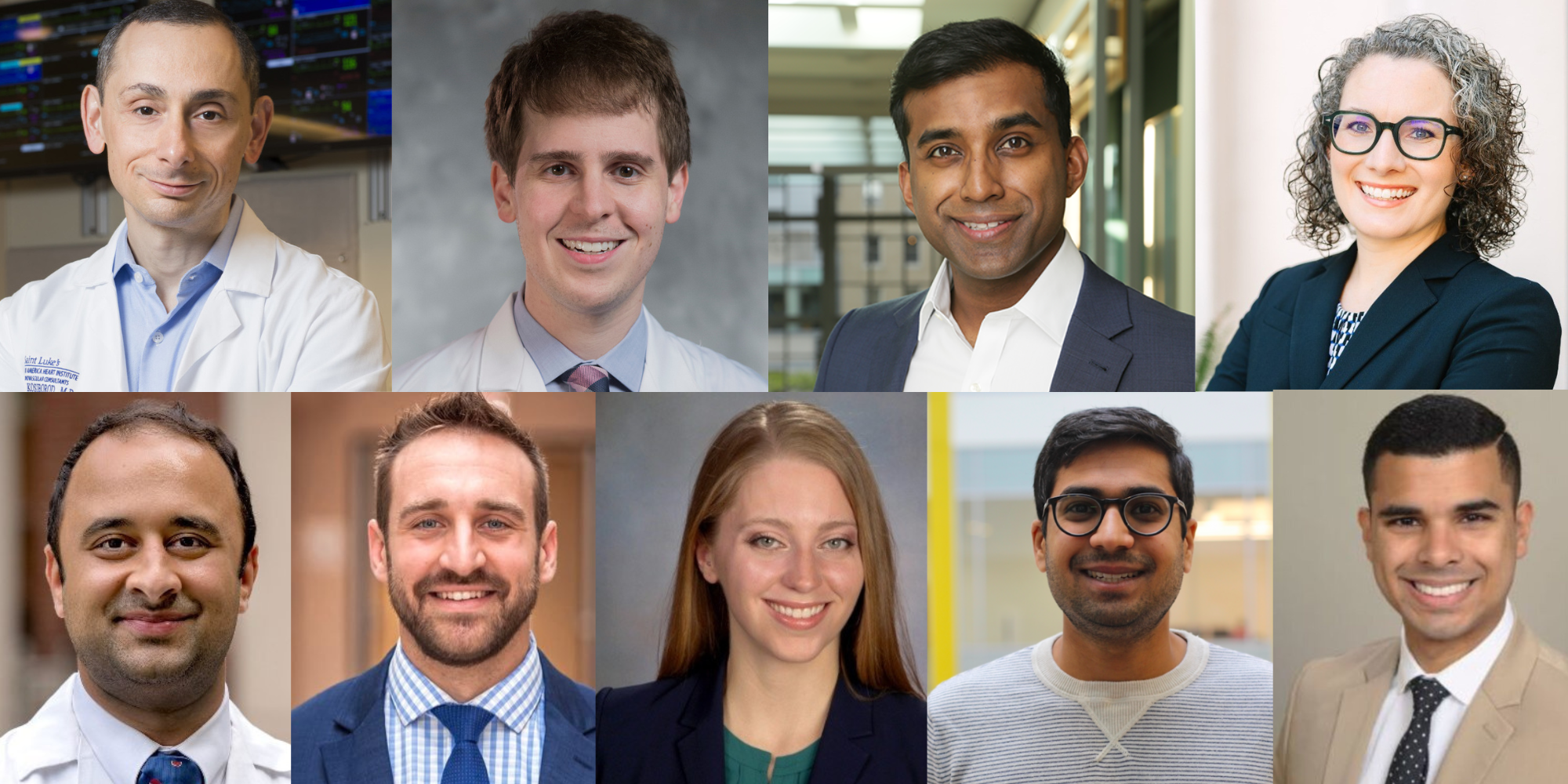
Our list of interview guests is as follows: Mikhail Kosiborod, MD, of Saint Luke's Mid America Heart Institute, Stephen Greene, MD, of Duke Clinical Research Institute, Muthiah Vaduganathan, MD,MPH, of Brigham and Women’s Hospital, Lauren Eyadiel, MMS, PA-C, of Wake Forest University School of Medicine, Ankeet Bhatt, MD, MBA, of Kaiser Permanente, Alex Hajduczok, MD, of Thomas Jefferson University, Jenna Skowronski, MD, of the University of Pittsburgh, Anand Shah, MD, MBA, of the University of North Carolina, and Jose Lopez, MD, of the University of Miami.
(Top Row; L to R) Mikhail Kosiborod, MD; Stephen Greene, MD; Muthiah Vaduganathan, MD, MPH; Lauren Eyadiel, MMS, PA-C
(Bottom Row; L to R) Ankeet Bhatt, MD, MBA; Alex Hajduczok, MD; Jenna Skowronski, MD; Anand Shah, MD, MBA; José López, MD
Kosiborod: I think the biggest story of 2023 is the STEP-HFpEF trial, and the role of targeting obesity as a treatment for HFpEF. For full disclosure, I am heavily involved in the STEP-HFpEF program, but I think that this trial has completely changed (and will continue to change) the way we view obesity in this patient group – from a coexisting condition to a root cause and a target for intervention. Not only will this ultimately have a significant impact on clinical practice, but it will also lead to many future research developments in this field, including hopefully testing many different pharmacologic interventions to improve a broad range of outcomes in patients with the obesity phenotype of HFpEF.
Greene: I think the biggest news in 2023 for heart failure is STEP-HFpEF with semaglutide. We have, for some time really, struggled with HFpEF and then we all celebrate when we had the SGLT2 inhibitors, which are a blockbuster advancement in themselves, but, this year, we have been talking about how many patients with heart failure care just as much, if not more, about their quality of life and functional status beyond things like hospitalization and death.
We now have a therapy that was tested in a very modest size clinical trial, with STEP-HFpEF having just over 500 patients, but really produced the largest, to my knowledge, quality of life improvement that we've ever seen in a heart failure trial. It goes to a population that needs all the help it can get. Patients with obesity and HFpEF who have very poor baseline quality of life, on average, and really don't have a lot of good therapeutic options as well beyond the SGLT2 inhibitor class, so we will still have to wait and see where the field of GLP-1 receptor agonists goes in terms of clinical outcomes. Again, STEP-HFpEF was safe and it resulted in major improvements in quality of life for a population that needs all the help we can get. I think this is a blockbuster result for our patients and it'll be interesting to see where this field goes next.
Vaduganathan: I think GLP-1 receptor agonism in heart failure with preserved ejection fraction has taken center stage. So, STEP-HFpEF, although was a modest sized trial, really puts forth a paradigm that will continue to be tested with multiple therapeutics and positions obesity as a modifiable factor in bending the trajectory of illness in patients with HFpEF. I think it also states that, until now, we haven't had individual phenotypes of HFpEF that were specifically targetable. Now, we have obesity-related HFpEF and we know in STEP-HFpEF that the drug can safely reduce weight and can safely improve health status to a large magnitude. At the American Heart Association meeting, we will hear the results from the landmark select trial, which was almost 18,000 patients with a large proportion of patients—about 4000—with coexisting heart failure. So, we will have a very good understanding if this drug further improves other clinical outcomes like hospitalizations and mortality.
Eyadiel: I think the headlining story and heart failure this year is, while we've, for the past couple years been seeing lots of data piling on the importance of 4 drug therapy, I think where we've really made some strides this year is number one: proving and standing behind the notion that these patients need these drugs, they're cost effective, and we need to do it in the hospital, right? Like the clinical inertia is going to be way worse, if the hospital discharge summary says consider as an outpatient. So, STRONG-HF was able to demonstrate that we really need to be getting these patients on those drugs while they're hospitalized.
So, all of that to say, I think that is a really important piece of heart failure news. In this current era, when we think about GDMT optimization, the other two things that I think have been really important, in terms of the literature in the heart failure community this year, are looking further into things that improve our patient's functional status—specifically with regards to IV iron therapy, and how to integrate that and implement that for our patients, with a focus in the outpatient setting where this can be a challenge.
Lastly, we've seen quite a bit of growth in the past year with the use of DCD [donated after circulatory death] donors in terms of the safety of this and the outcomes of this as compared with how we've traditionally practice, which in turn is going to allow us in the future to utilize more organs. And I think that that's really important for our patients who do go on to new cardiac transplantation.
Bhatt: I'm incredibly optimistic about heart failure therapy, I think there are a number of things that are in the pipeline, that have the ability to totally rethink how we're going to be successful in both discovery and implementation science in heart failure. There will be new combination therapies coming out, we still have lots of excitement and interest in novel mineralocorticoid antagonism as well, but this year, I think has really been a resetting year around understanding implementation. We've seen now a number of implementation studies that have come out aimed at improving guideline directed medical therapy and I think this is critically important, as we're starting to evaluate new therapies, such as GLP-1 receptor agonists in the STEP-HFpEF trial. I think it is an exciting new paradigm and we really need to get implementation right so that, as these new therapies undergo large phase three randomized clinical trials in the years to come, we are ready to be able to get these to patients at scale and very quickly.
Hajduczok: Well, I'm sure that everybody has already said STEP-HFpEF for this so I will take a slightly different angle. We'll start with probably something that was big in the news in 2022, which was xenotransplant, which is still going on and I think that that's going to be important, but on the similar topic of transplant, I think that the New England Journal of Medicine article where Jacob Schroeder, MD, was the lead author showed in a randomized fashion that there was no difference in outcomes between DCD and non-DCD hearts. This expanded the donor pool by about 30%, which is huge for our patients. It means shorter waitlist times and it means better outcomes in the hospital. We'll get more of the longer-term data with DCD in the in the coming years, but I think that it'll be really help create a paradigm shift to really get more people transplanted and give them their lives back.
Skowronski: As this is my first HFSA, personally, it's been outstanding as a trainee in a year where the field is really concerned about the number of people going into heart failure to get to meet people, feel the enthusiasm, and get to talk to them. So, that's been wonderful.I think that we are having more conversations about cardio obstetrics. At this point, there are sessions regarding it and we had a number of wonderful experts that are here to discuss it. So, whenever I look at this HFSA and I look back at it, I'll not only think of it as my first HFSA that I got to experience, but also a place where I was really able to solidify what I want to go into in heart failure and how I want to practice and see role models that are doing just that.
Shah: I think a lot of it builds off a lot of the prior work and data we have were, as you said, a "quieter" year, in terms of no like big as big blockbuster meds that we know are going to change mortality or outcomes, but I think that led to what the new trend and focus on heart failure has been is we have all these medications and interventions that we know work. The next big challenge is how do we make sure all of our patients can actually benefit from it? Because it's one thing to wave around and say, "Hey, we have all these medications", but if the patients aren't taking them or if they can't have access to them, then it really doesn't do us or our patients much good. So, how do we really translate this into clinical practice and have it reach the patients?
Lopez: The headline for 2023, I think it's SGLT2s and now other drugs, such as GLP-1s, are like wonder drugs and they have been shown to help even HFpEF, which has been the toughest part of the heart failure tackle because there were no therapies for it. Another study I liked a lot was the recent study published by the Journal of Cardiac Failure about heart failure statistics, I was very excited to see that—it was a great effort. So, I think STEP-HFpEF and the HF Stats were my favorite takeaways from this year.
Editor’s note: Some transcripts have been edited for grammar and clarity.





