Hypertension Complicated by Heart Disease
What is the optimal treatment for hypertension when the patient also has Afib, CAD, or heart failure?
Recently we looked at the treatment of hypertension in the context of chronic kidney disease. This time, let’s look at hypertension in persons who have comorbid heart disease, specifically atrial fibrillation (AF), coronary artery disease (CAD), and systolic heart failure. The quiz is a quick check on what you know about important co-managment.
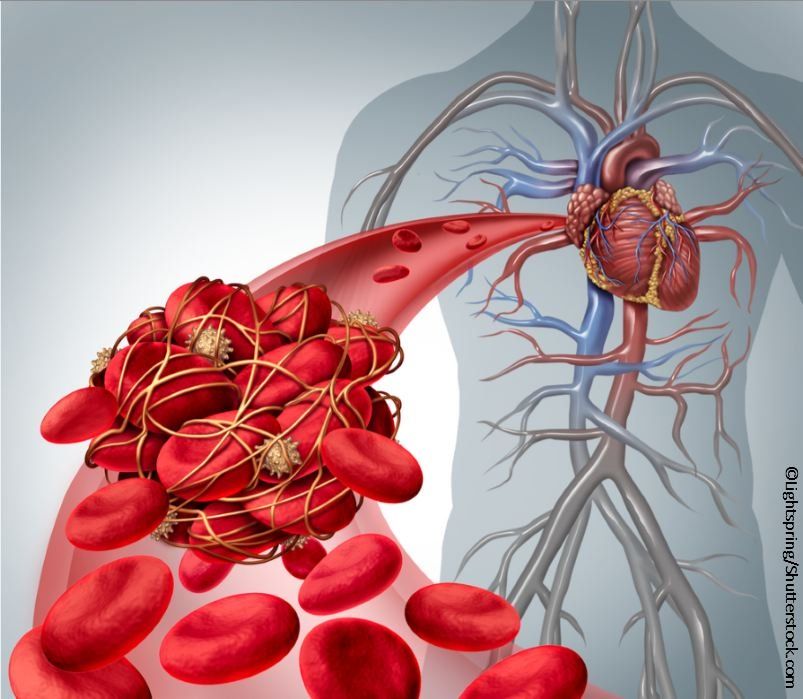
What does AF have to do with high blood pressure?
In the Women’s Health Study, 34,221 women were followed for the development of incident AF.1 The cumulative incidence of AF increased across a continuum of rising blood pressures. The higher the blood pressure, even if it was not at a level requiring therapy, the higher the incidence of AF. Unfortunately, hypertension and AF often coexist and are synergistic in causing morbidity: hypertension is associated with left ventricular hypertrophy, impaired ventricular filling, left atrial enlargement, and slowing of atrial conduction velocity-all changes that are conducive to atrial arrhythmia.
1. Regarding the relationship of AF and hypertension, which of the following is/are true?
A. When patients with AF are optimally anticoagulated, hypertension is still independently associated with a higher risk of stroke.
B. In recent clinical trials of novel oral anticoagulants (NOACs) enrolling AF patients, 80-90% of individuals with AF also had hypertension.
C. In patients with AF who are not anticoagulated, hypertension as a comorbidity does not affect the risk of stroke.
D. A and B
E. B and C
Answer and discussion>>
Answer: D. A and B are true
In persons with AF who are anticoagulated, the risk of stroke is increased with coexisting hypertension.2 The trials proving the efficacy of the NOACs in preventing strokes demonstrated that AF is accompanied by hypertension as a comorbidity almost universally.2 If AF is not approached both with anticoagulation and hypertension control, a risk of stroke is significant.2 Bottom line, anticoagulation in AF patients must be accompanied by blood pressure control as the standard of care to prevent strokes.
What’s different about antihypertensive therapy in patients who have CAD?
2. Which of the following choices is/are correct (choose as many as appropriate)?
A. Despite fewer indications for beta blockers as antihypertensive therapy in patients without heart disease, beta blockers are the first choice in patients who have both hypertension and CAD.
B. It is suggested that prescribing atenolol for hypertension in patients with coexisting CAD is not appropriate. Recommended agents are cardioselective beta blockers without sympathomimetic activity such as metoprolol or bisoprolol.
C. Diuretics and ACEI/ARBs are second line agents for hypertension when beta blockers alone do not reach target blood pressures.
D. If patients with heart disease are at risk for an acute coronary syndrome or stroke, their target BP should be 130/80 mmHg.
Answer and discussion>>
Answer: All are correct
The 2015 ACC/AHA/ASH guidelines are explicit: beta blockers are the first choice for antihypertensive therapy in patients with coronary disease and hypertension.3,4 However, results of a review of studies in patients with hypertension and CAD4 led review authors to recommend that atenolol not be the beta blocker of choice.4 The same caveats apply to its choice over other antihypertensive agents in general, ie, in patients with hypertension who do not have heart disease (based on data from studies such as LIFE, where atenolol performed poorly vs other antihypertensive agents, with regard to strokes and other outcome measures.)4,5
On the topic of hypertension therapy in patients with systolic heart failure:
Is the following statement regarding beta blockers in patients with heart failure true or false?
The beta blockers that demonstrated a mortality benefit in patients with heart failure are metoprolol (MERIT-HF); carvedilol (COPERNICUS); bisoprolol (CIBIS-II); nebivolol (SENIORS).
A. True
B. False
Answer and discussion>>
Answer: A. True; all have demonstrted mortality benefit in patients with heart failure.3
References
1. Conen D, Tedrow UB, Koplan BA, et al. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation 2009; 119:2146-2152. http://circ.ahajournals.org/content/119/16/2146.long
2. Rao MP, Halvorsen S, Wojdyla D, et al. Blood pressure control and risk of stroke or systemic embolism in patients with atrial fibrillation: Results from the Apixaban for reduction in stroke and other thromboembolic events in Atrial Fibrillation (ARISTOTLE) Trial. J Am Heart Assoc. 2015; e002015 doi: 10.1161/JAHA. 115.002015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4845276/
3. Rosendorff C. Treatment of hypertension in patients with coronary artery disease: A case-based summary of the 2015 AHA/ACC/ASH scientific statement. Am. J. Med 2016;129:372-378. https://www.ncbi.nlm.nih.gov/pubmed/?term=Am.+J.+Med+2016%3B+129%3A372-378.
4. Aronow WS. Current treatment of hypertension in patients with coronary artery disease recommended by different guidelines. Expert Opin Pharmacother. 2016 17:205-215. http://www.tandfonline.com/doi/abs/10.1517/14656566.2015.1091881?journalCode=ieop20
5. Carlberg B, Samuelson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004;364:1684-1689. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(04)17355-8/abstract