Injection and aspiration of the finger joints
The hand-the chief sensory organ of touch-performs grasping and fine manipulations that are essential for dexterity and performance of activities of daily living. Critical to maintaining these roles is preservation of finger joint function. For patients who present with finger pain or swelling, a comprehensive plan of evaluation and management may require diagnostic aspiration or therapeutic injection or both.
The hand-the chief sensory organ of touch-performs grasping and fine manipulations that are essential for dexterity and performance of activities of daily living. Critical to maintaining these roles is preservation of finger joint function. For patients who present with finger pain or swelling, a comprehensive plan of evaluation and management may require diagnostic aspiration or therapeutic injection or both.
Finger joints may be affected by the full array of arthritides, focal or systemic and inflammatory or noninflammatory. Although specific diseases often affect certain joints (eg, the distal interphalangeal [DIP] joints in osteoarthritis [OA] or the metacarpophalangeal [MCP] joints in rheumatoid arthritis), there is enough overlap between diseases with regard to their site of joint involvement (eg, gouty arthritis in a DIP joint with nodal OA) that the clinician should be comfortable with performing arthrocentesis in the fingers as a part of patient assessment and treatment.
In a previous article ("Injection of the first carpometacarpal joint," The Journal of Musculoskeletal Medicine, June 2008, page 295), we discussed arthrocentesis of the carpometacarpal joint of the thumb. In this article, we describe our approach to aspirating and injecting the MCP and IP joints of the fingers.
Suggested supplies
•1-mL syringe with 0.5 to 1 mL of 1% lidocaine for local anesthetic (or ethyl chloride or both).
•1-mL syringe with 0.25 mL of 1% lidocaine mixed with 0.25 mL of a triamcinolone-based corticosteroid, 40 mg/dL (or other fluorinated corticosteroid equivalent). Given the small joint size, mixing lidocaine with the corticosteroid is optional.
•3- to 5-mL syringe for joint aspiration.
•0.5- to 0.625-inch, 25- to 26-gauge needles for injection of both anesthetic and corticosteroid/anesthetic mixture and 23- to 25-gauge needles for aspiration.
•Alcohol wipes, povidone-iodine, or chlorhexidine for sterilization.
•Sterile hemostat (optional).
•Nonsterile or sterile gloves.
•Gauze pads and an adhesive bandage.
•Appropriate tubes and slides for synovial fluid analysis.
Surface anatomy
Joint lines of the MCP and IP joints of the fingers are best palpated in slight flexion on either side of the dorsal, midline extensor tendon apparatus. Passive flexion and extension of the joint during palpation may facilitate this identification. Note that the sulcus of the MCP joint line is located at almost the distal end of the metacarpal head ("knuckle").
IP joint lines typically are more difficult to identify. However, a careful examination should identify an entry point that will ensure that the needle tip will come to rest under the joint capsule.
Patient position and needle placement
The patient should be seated in a comfortable chair next to the examination table with the affected hand and forearm resting palmar surface down on the table for stability. Identify a point of needle entry on the joint line on either side of the dorsal extensor tendon between it and the midline neurovascular bundle running along either side of each finger.
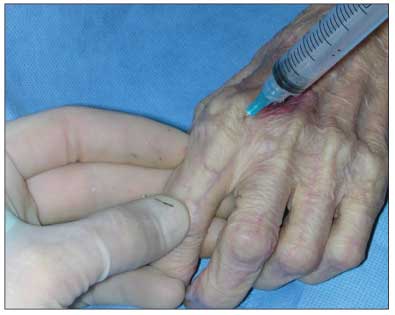
Figure – Injection of the left second metacarpophalangeal joint is depicted in this cadaver photograph. With the joint flexed and traction applied with the physician's noninjecting hand, the needle is entered into the joint between the extensor tendon and the ulnar-side neurovascular bundle. During successful injection, joint capsular distention can be palpated on the volar surface with the noninjecting hand, as shown.
ProcedureMCP joint: After sterilization and application of local anesthetic, with the joint flexed and mild axial traction applied, insert the needle toward the midline of the finger. Direct the needle in a slight cephalad direction to account for the natural cupping of the base of the proximal phalanx (Figure). Application of slight pressure against the syringe plunger during injection should make the joint bulge slightly.
IP joint: After sterilization and application of local anesthesia, with the joint flexed and mild axial traction applied, insert the needle toward the midline of the finger. Direct the needle more perpendicular to the skin in contrast to entering the MCP joint as noted above. Slight pressure against the syringe plunger during injection should make the joint bulge slightly.
Pearls
•The operator's noninjecting hand may be used to both distract the joint and palpate for signs of a successful injection. Use the fourth and fifth fingers to grasp and slightly pull traction and flex the joint, use the thumb nail to identify the joint line, and place the second or third finger or both on the volar aspect of the joint to palpate for joint capsular distention during injection.