Article
Insured Millennials Report Significantly More Cases Since 2014
Author(s):
A new study of 55 million insured young adults in the US found that major depression, type 2 diabetes, and other conditions are becoming more prevalent among them.
An assessment of commercially insured Americans has found that the rates of serious conditions including major depression, type 2 diabetes (T2D), and hypertension have risen significantly among millennials from 2014 to 2017.
In an age group-specified study of common condition claims made to Blue Cross Blue Shield (BCBS) over 4 years, investigators reported that insured patients born between 1981-1996 may be unhealthier than older generations were at their age.
The 26th study from The Health of America Report—a collaboration between BCBS and Blue Health Intelligence (BHI) that used the data of 55 million insured millennial Americans—found what BCBS Executive Director of Research & Analytics Brian Harvey called “disturbing results” for the current state of younger generations’ health.
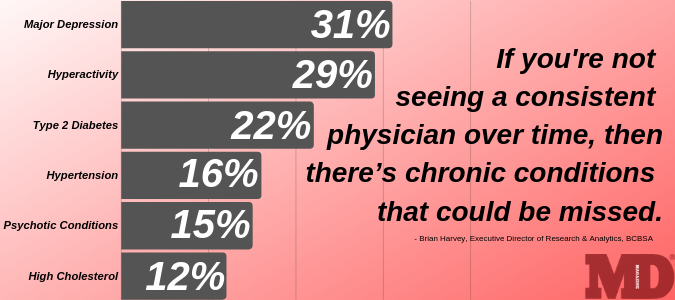
Harvey and his colleagues conducted a comparison of reported case rates among millennials in 2014 and 2017. Among the 10 conditions designated by the BCBS Health Index to carry the most adverse health impact, 8 had increased in prevalence among millennials by 10 percentage points or more since 2014.
The greatest increase was observed in cases of major depression (31%), which rose from 3.8% of millennial Americans to 5% in those 4 years. As per the index—which accounts for each conditions’ reduction in future patient healthy years—major depression carries the greatest risk of adverse health effects among millennials.
The approximate 200 conditions included in the BCBS index comprise more than 98% of the cases filed by insured patients, Harvey explained.
Other cases to increase by 10 percentage points or more included:
- Hyperactivity (29%)
- T2D (22%)
- Hypertension (16%)
- Psychotic conditions (15%)
- High cholesterol (12%)
- Crohn’s disease/Ulcerative colitis (10%)
- Substance use disorder (10%)
Harvey told MD Magazine® that the rise of behavioral health condition cases were unsurprising, given that younger generations are more likely to face greater risk of those than most physical conditions.
He expressed far greater concern for the jump in T2D, hypertension, and high cholesterol rates—coupling the findings with evidence showing that the same age group is far less likely to consistently see a primary care physician, meaning these chronic conditions can go unchecked for far too long.
“Part of the challenge there is, if you’re not seeing a consistent physician over time, then there’s chronic conditions that could be missed,” Harvey said. “Crohn’s and ulcerative colitis are 2 debilitating conditions that are difficult to treat, and there’s been 10% growth in the millennial population. Many of these patients will be dealing with it for the rest of their lives.”
In comparing the high-risk condition prevalence rates among millennials aged 34-36 in 2017 to the rates among members of Generation X in 2014—who were aged 34-36 years old at that time—the younger generation fared markedly worse in cases of hyperactivity (37%), T2D (19%), and major depression (18%), among others.
A study published last week from Stony Brook University’s Renaissance School of Medicine showed that provisions to the Affordable Care Act (ACA) in 2014 aimed to broaden insurance coverage in the US, and has since been associated with decreased rates of uninsured hospitalizations and emergency department visits.
When asked whether such provisions to bolster insurance rates could have influenced the boom of condition cases made by millennials from 2014-2017, Harvey said his team didn’t witness a significant change in insured rates among the age group during that time span. He added that the comparison of condition cases among similarly-aged millennials and patients from Generation X solidified the team’s beliefs these findings are significant.
“The health status of millennials will likely have substantial effects on the American economy over the next two decades—including workplace productivity and healthcare costs,” investigators concluded. “BCBS is partnering with Moody’s Analytics to forecast how the health of millennials will impact the future economy, with results highlighted in an upcoming BCBS Health of America report.”





