Managing Urticaria: New Guidelines and Beyond
Clinicians have several guidelines, algorithms, and other tools at their disposal that can assist them in the differential diagnosis and management of chronic urticaria.
During the American Academy of Allergy, Asthma and Immunology’s 2015 annual conference in Houston, TX, Marcus Maurer, MD, from the University of Berlin, discussed the most recent EAACI/GA2LEN/EDF/WAO guidelines for the treatment of chronic urticaria (CU).
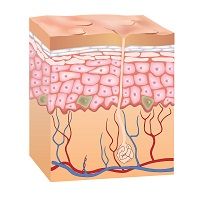
He noted that patients with CU may present with itchy wheals or angioedema. In some cases, patients may present with both wheals and angioedema. Maurer noted that each year, experts from around the world reunite in Berlin, Germany, to discuss new recommendations on how to treat the disease.
While discussing approaches to the diagnostic workup of patients with CU, Maurer said that first it is important to rule out other diseases. He also noted that the presence of severe inflammation or inflammatory diseases must be investigated, and clinicians should measure the activity and impact of the disease. At this point, the cause of CU is not under investigation.
To rule out other diseases, Maurer presented an algorithm to guide clinicians in the diagnosis. This algorithm starts with the main symptoms of the disease, wheals and angioedema, and leads to six possible diagnosis, two of them being urticaria, either spontaneous or inducible. Two markers of inflammation must be checked in the blood so as to rule out severe inflammation: erythrocyte sedimentation rate (ESR) and C-Reactive protein (CRP).
In order to evaluate the activity and impact of the disease, several scores are available, including the urticaria activity score (UAS) and the urticaria control test (UCP). These questionnaires are available online and are completed by the patients. These scores help clinicians follow their patients’ diseases and guide the selection of appropriate therapies. According to Mauer, the search for the cause of CU should not be performed in every patient. Only those with suggestive clinical history and with severe and long-standing lesions should be investigated.
Next, Maurer presented the guidelines for diagnosing patients with chronic inducible urticaria. Similarly to CU, three initial steps are necessary when evaluating affected patients: First, exclude other diseases; second, exclude severe inflammation, and third; confirm the triggering agent and measure its threshold. He then presented the most common tools used to evaluate triggers and threshold.
Regarding treatment of CU, Maurer emphasized that there is no specific treatment, and that prevention is the key factor. In general, the international guidelines suggest the use of second-generation antihistamines as the first step. If symptoms persist, the dose of these antihistamines may be elevated. Maurer highly discouraged the combination of antihistamines or the use of sedating antihistamines. Another option to treat patients with CU is the use of anti-IgE drugs. Although CU is not considered an allergic disease, patients have increased expression of IgE and may benefit from the use of these drugs. Indeed, the use of omalizumab, an anti-IgE drug, in a multi-center placebo-controlled trial reduced chronic spontaneous urticaria activity in 70% of participants. The mechanisms involved in this protective effect seem to be the binding of the drug to IgE in the blood and skin, the down regulation of IgE receptors, and the decrease in the number of mast cells.
Finally, Mauer informed the audience that the response to this treatment is variable and seems to be dependent on the dosage used, intervals, and the severity of the disease. Further studies are necessary to improve the safety and efficacy of anti-IgE therapy.