No Clear Evidence Acupuncture Provides Benefit in Chronic Spontaneous Urticaria
A randomized trial examining acupuncture in people with CSU suggests use of acupuncture could improve UAS7 scores in these patients, but investigators noted this failed to reach the threshold for significance.
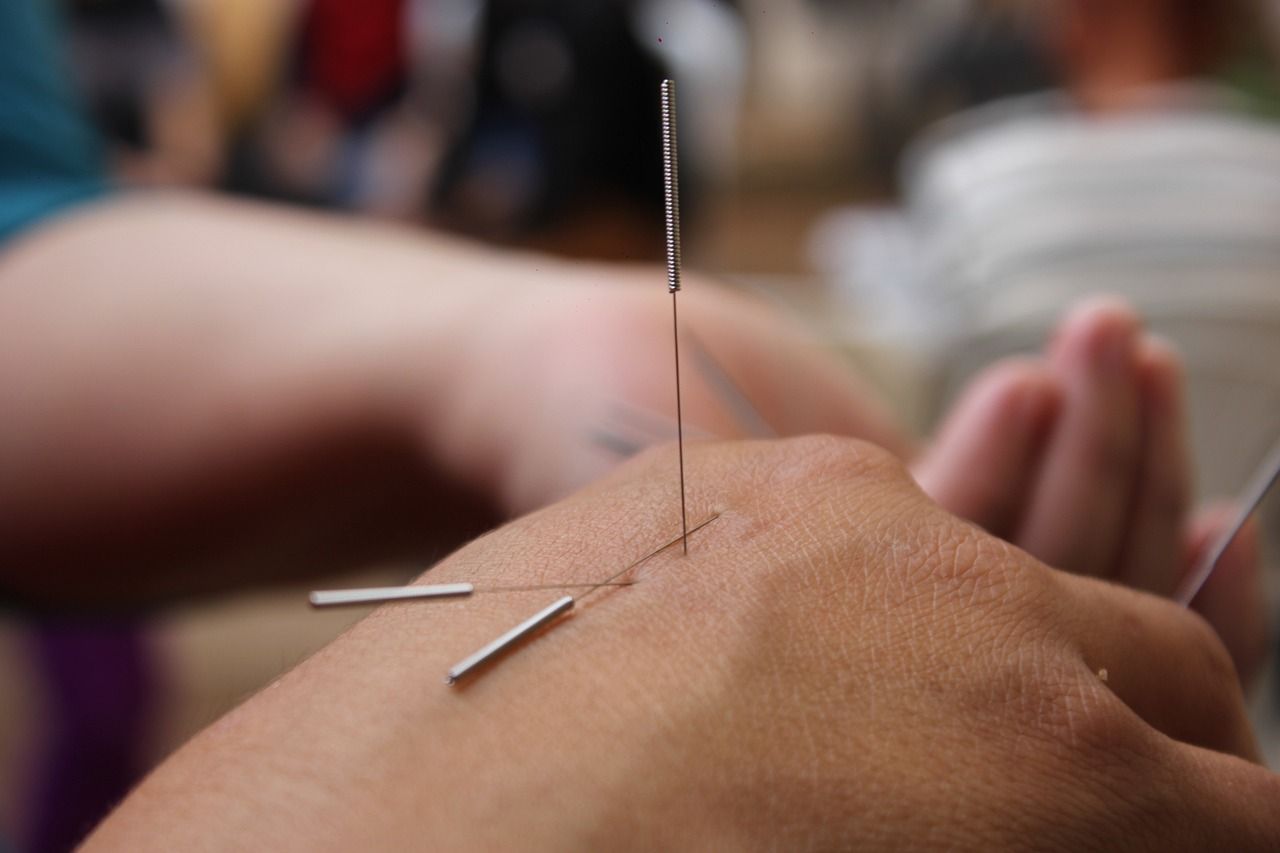
Credit: Jorge Paredes; Pixabay
A randomized controlled trial of more than 300 participants with chronic spontaneous urticaria is providing new insight into the effects of acupuncture on disease symptoms and quality of life.
A trial comparing acupuncture against sham acupuncture and a waitlist control, results of the trial, which used the Weekly Urticaria Activity Score (UAS7) to assess the effects of treatment, found acupuncture was associated with a greater improvement in UAS7, but investigators pointed out this did association did not reach the threshold for statistical significance.1
“The results of the primary and secondary outcomes suggested a greater improvement in [chronic spontaneous urticaria] symptoms in participants who received 16 sessions of acupuncture over 4 weeks than in those who received sham acupuncture or were in a waitlist control group, although clinical significance is unclear,” wrote investigators.1
The result of autoimmune mechanisms, chronic spontaneous urticaria is defined as the occurrence of widespread wheals, angioedema, or both, for more than 6 weeks and is estimated to affect 1 to 2% of the general population, with a higher prevalence in female patients, and is more frequent patients over 20 years of age.2
Citing previous evidence suggesting acupuncture could inhibit peripheral and central transmission of pruritus, a team led by Ying Li, MD, PhD, of the Chengdu University of Traditional Chinese Medicine, sought to build on the existing evidence base surrounding use of acupuncture. In the current trial, investigators randomized patients in a 1:1:1 ratio to receive acupuncture, sham acupuncture, or waitlist control over an 8-week study period, which consisted of 4 weeks of treatment and 4 weeks of follow-up.1
Patients in the trial were recruited from the outpatient departments of 3 tertiary hospitals in 3 different cities in China. All patients were recruited through advertisements, questionnaires, and hospital posters and underwent screening by dermatology specialists screened participants for eligibility at each participating center.1
Those randomized to acupuncture received 10 sessions in the first 2 weeks and an additional 6 sessions in the subsequent 2 weeks, with 16 sessions in total. These sessions lasted 30 minutes. Those in the sham group received the same number of sessions and were treated with nonpenetrating acupuncture at sham acupuncture points.1
The primary outcome of interest for the trial was the mean change from baseline to week 4 in UAS7. The trial also included multiple secondary outcomes, such as itch severity scores, self-rated improvement, and Dermatology Life Quality Index scores.1
Upon analysis, results suggested the mean change in UAS7 from baseline to weekly 4 was greater among those in the acupuncture group (-8.2; 95% Confidence Interval [CI], -9.9 to -6.6) than those in the sham acupuncture (-4.1; 95% CI, -5.8 to -2.4) and the waitlist control group (-2.2; 95% CI, -3.8 to -0.5). Investigators pointed out the mean differences seen between acupuncture and sham acupuncture (-4.1; 95% CI, -6.5 to -1.8) and acupuncture and waitlist control (-6.1; 95% CI, -8.4 to -3.7) did not meet the threshold for minimal clinically important difference.1
When assessing safety, results indicated 13.6% of patients in the acupuncture group and none in the other groups reported adverse events. However, investigators noted all adverse events occurring in the trial were considered mild or transient.1
Investigators noted multiple limitations to consider when interpreting results from the trial. These included a relatively short study period, adoption of an intensive acupuncture treatment scheme, and comparing acupuncture against no, or only occasional, antihistamine use.1
“Although the acupuncture treatment studied was fairly intensive, including a total of 16 sessions over 4 weeks, it is noteworthy that the effect of acupuncture persisted for 1 month after the end of acupuncture treatment,” investigators added.1 “Further studies should examine whether similar effects may be found with fewer acupuncture sessions.”
References:
- Zheng H, Xiao XJ, Shi YZ, et al. Efficacy of Acupuncture for Chronic Spontaneous Urticaria : A Randomized Controlled Trial [published online ahead of print, 2023 Nov 14]. Ann Intern Med. 2023;10.7326/M23-1043. doi:10.7326/M23-1043
- Murdaca G, Paladin F, Borro M, Ricciardi L, Gangemi S. Prevalence of Autoimmune and Autoinflammatory Diseases in Chronic Urticaria: Pathogenetic, Diagnostic and Therapeutic Implications. Biomedicines. 2023;11(2):410. Published 2023 Jan 30. doi:10.3390/biomedicines11020410