No Increase in Fracture Risk from SGLT2 Inhibitor Use, Study Finds
A propensity score-matched analysis comparing fracture risk associated with the initiation of SGLT2 inhibitors versus GLP-1RAs or DPP-4 inhibitors indicates use of SGLT2 inhibitors was not associated with an increase in risk of fractures in older patients with type 2 diabetes.
New research from investigators at Brigham and Women’s Hospital and Harvard Medical School suggests use of SGLT2 inhibitors was not associated with an increased risk of fracture in older adults with type 2 diabetes compared to other therapies.
A propensity score-matched analysis of data from a cohort of nearly 500,000 Medicare beneficiaries with type 2 diabetes and no history of fracture, results of the study demonstrate initiating treatment with an SGLT2 inhibitor was not associated with an increased risk of fracture compared to initiating treatment with a dipeptidyl peptidase 4 inhibitor (DPP-4i) or a glucagon-like peptide 1 receptor agonist (GLP-1RA).
“In this nationwide Medicare cohort, initiating an SGLT-2i was not associated with an increased risk of fracture in older adults with T2D compared with initiating a DPP-4i or GLP-1RA, with consistent results across categories of frailty, age, and insulin use. These findings add to the evidence base evaluating the potential risks associated with SGLT-2i use for older adults outside of randomized clinical trials,” wrote investigators.
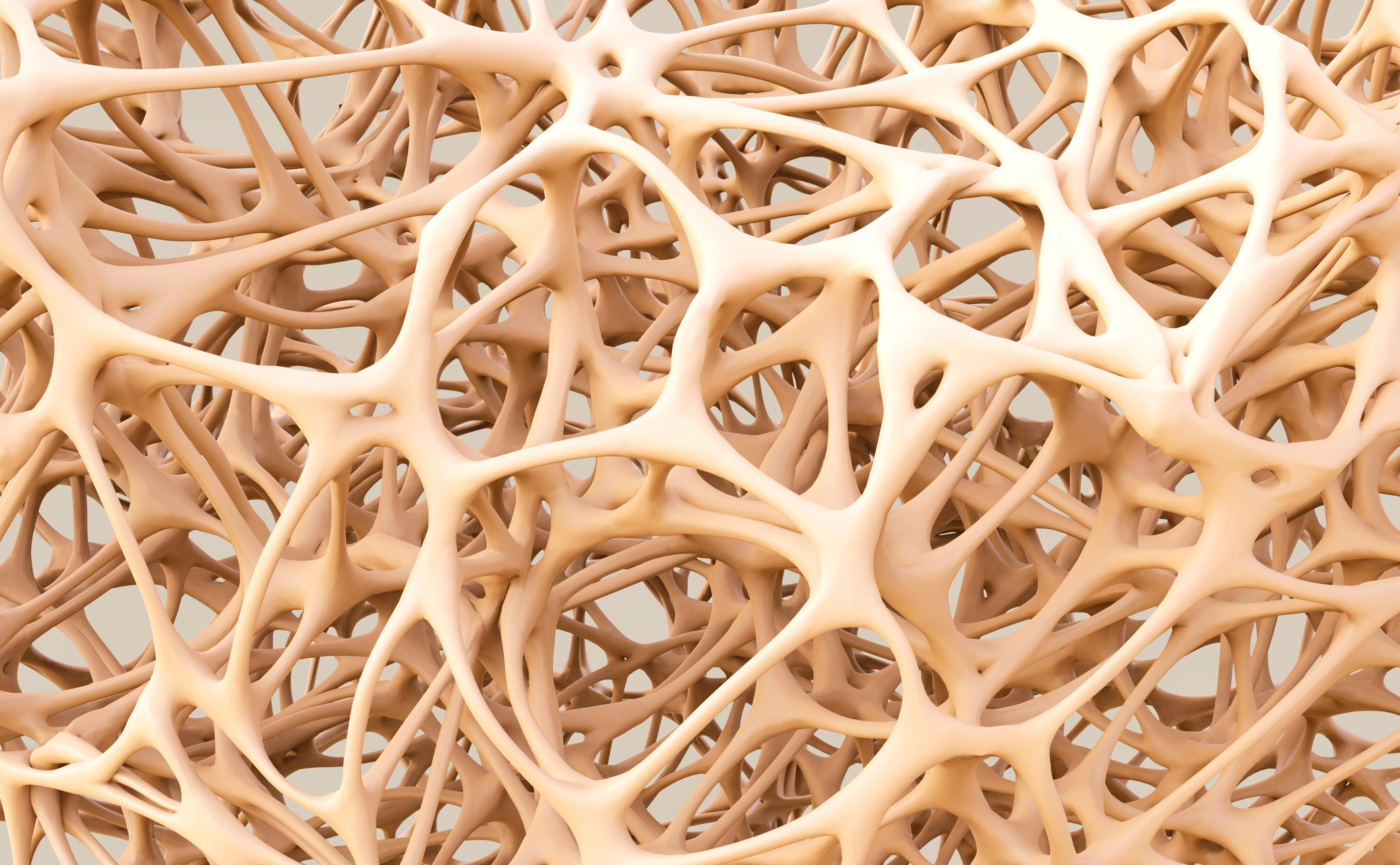
Although SGLT2 inhibitors have become the center of discussion for clinicians with an interest in cardiometabolic health in recent years, some have raised concerns over the safety profile of these agents in real-world settings. With former studies implicating a potential impact on bone health, a team of 9 Harvard Medical School-based investigators sought to investigate the effects of SGLT2 inhibitors on fracture risk in comparison to other therapies leveraging Medicare fee-for-service data.
Searching Medicare fee-for-service data from April 2013 to December 2017, investigators identified a cohort of 466,933 patients aged 66 years of age or older with type 2 diabetes and no history of fracture for potential inclusion in their study. For inclusion in the study, patients needed to be newly prescribed 1 of the 3 aforementioned therapy classes during the study period. Investigators noted 66 years was chosen as the lower cutoff for age so patients would have at least 1 year of Medicare eligibility before cohort entry.
Exposures of interest for the study were defined as new use of any SLGT2 inhibitor, GLP-1RA, or DPP-4i. The SGLT2 inhibitors included in the study were canagliflozin, dapagliflozin, and empagliflozin. The DPP-4 inhibitors included in the study were alogliptin, linagliptin, saxagliptin, and sitagliptin. The GLP-1 receptor agonists included in the study were albiglutide, dulaglutide, exenatide, liraglutide, lixisenatide, and semaglutide. The primary outcome of interest for the study was a composite of nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention within 30 days. Secondary outcomes of interest included incidence of falls, hypoglycemia, and syncope.
After the application of 3-way propensity score matching, investigates identified 45,889 matched sets of patients, including a total of 137,667 patients in the final study cohort. This population had a mean age of 72 (SD, 5) years and 47% were men. Investigators planned to use multivariable Cox proportional hazards regression models to estimate hazard ratios for SFGLT2 inhibitor use compared with DPP-4 inhibitors and GLP-1RA use. Additionally, Kaplan-Meier curves were used to visualize fracture risk over time.
Upon analysis, there were no differences observed in the risk of fracture for SGLT2 inhibitor users when compared to DPP-4i users (HR, 0.90; 95% CI, 0.73-1.11) or GLP-1RA users (HR, 1.00; 95% CI, 0.80-1.25). When assessing secondary outcomes, results indicated the risk of falls (HR, 0.82; 95% CI, 0.77-0.87) and hypoglycemia (HR, 0.75; 95% CI, 0.67-0.84) were lower in SGLT2 inhibitor users compared against matched DPP-4i users but no difference was observed for syncope. Investigators noted no difference in falls, hypoglycemia, or syncope for SGLT12 inhibitor users compared with GLP-1RA users.
This study, “Association of Sodium-Glucose Cotransporter–2 Inhibitors With Fracture Risk in Older Adults With Type 2 Diabetes,” was published in JAMA Network Open.