Study Finds Hydroxyurea Dose Escalation Lowers Stroke Risk in Children with Sickle Cell Anemia
A study in the Dominican Republic assessed the use of dose escalation of hydroxyurea for children in a single hospital with sickle cell anemia.
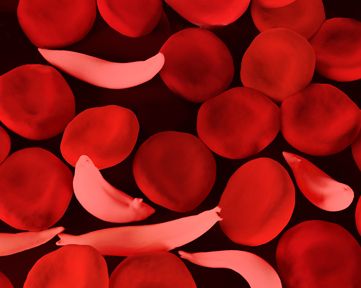
The Stroke Avoidance for Children in República Dominicana (SACRED) trial found that children with sickle cell anemia (SCA) and conditional transcranial Doppler (TCD) velocities saw positive results after hydroxyurea treatment at maximum tolerated dose (MTD).
SCA is noted by the trial investigators as common across the Caribbean, though lack of proper treatments has led to higher morbidity with the condition.
The SACRED trial was led by Rosa M. Nieves, MD, from the Robert Reid Cabral Hospital in Santo Domingo, Dominican Republic. Trial data was presented at the American Society of Hematology (ASH) Annual Meeting and Exposition.
“We designed a prospective clinical trial, Stroke Avoidance for Children in REpública Dominicana (SACRED), to build local capacity for clinical research and transcranial Doppler (TCD) screening, and to use hydroxyurea with dose escalation to maximum tolerated dose (MTD) to reduce the incidence of primary stroke in high-risk children with SCA,” Nieves and colleagues wrote. “We now report the primary results of the SACRED trial.”
Background
The investigators conducted a single center, open-label, prospective, phase 2 trial at the primary pediatric hospital in Santo Domingo, known as the Hospital Robert Reid Cabral. They recruited medical school graduates to be trained with TCD and complete several examinations, so that they could work for at least a year on the trial.
The team recruited pediatric SCA patients being given care at the hospital who were screened for TCD. They offered hydroxyurea for primary stroke prophylaxis to those children reporting conditional time-averaged mean velocities (TAMV 170-199 cm/sec). They referred children with abnormal TAMV (≥200 cm/sec) for monthly transfusions built for stroke prevention.
The investigators rescreened patients with normal TCD velocities at 12 months later and then 24 months later. Study participants were all given 20 mg/kg/day until after month 6, where they were then escalated to MTD based on blood count measures.
Findings
The study results found that of the 77 children eligible for hydroxyurea, due to TCD velocity development, escalation to MTD was achieved in 80% (59) of the patients. A stable dose was established for the remaining 20% of pediatric patients.
After 24 months of hydroxyurea, the investigators reported that the average dose was 25.8 ± 6.1 mg/kg/day, adding that sustained treatment effects included Hb = 9.0 ± 1.5 g/dL, HbF = 30.2 ± 13.6%, and ANC = 4.3 ± 2.1 x 109/L (all P<0.0001).
The average TCD value for patients by 24 months was found to be 157 ± 22 cm/sec in the primary endpoint analysis. This data demonstrated sustenance of a 23 ± 21 cm/sec decline from baseline, with 65% of the patients going back to normal TCD velocities.
“In the prospective SACRED trial, local capacity building in the DR led to a robust screening and treatment program to prevent primary stroke,” they wrote. “Children with SCA and conditional TCD velocities were successfully treated with hydroxyurea at MTD with excellent laboratory effects, lowering of TCD velocities, and no clinical strokes.”
The study, “Hydroxyurea with Dose Escalation to Reduce Primary Stroke Risk in Children with Sickle Cell Anemia in Dominican Republic: The Sacred Trial,” was presented at ASH 2022.