Suboptimal Management of Cardiovascular Risk Factors: Whose Fault Is It?

Leslie Cho, MD, FA CC
REVIEW
Driscoll A, Beauchamp A, Lyubomirsky G, Demos L, McNeil J, Tonkin A. Suboptimal man- agement of cardiovascular risk factors in coronary heart disease patients in primary care occurs particularly in women [published online ahead of print June 1, 2011]. Intern Med J. doi:10.1111/j.1445-5994.2011.02534.x.
There have been numerous studies showing the benefit of cho- lesterol lowering, blood pressure control, and healthy lifestyle in primary and secondary prevention of cardiovascular disease. Yet in study after study, conducted in different popu- lations over many years, it has been shown that cardiovascular risk factors are undertreated.1,2
As all developed countries struggle with rising health care costs and grow- ing elderly populations, it is crucial that we understand why our patients are being undertreated, and how to make changes in practice so that all patients who are at risk are treated optimally. The study by Driscoll et al sought to compare how well female patients with coronary heart disease (CHD) are controlled for their risk factors in a primary care setting in Australia by comparing their management with that recommended in guidelines and that provided to male patients.3
Study Details
The authors used a chronic disease management program (mdCare, developed by Merck, Sharp, and Dohme Australia) that is available to general practitioners (GPs) in Australia to compare management of patients with CHD. Of the 6000 GPs approached, 1258 were enrolled in the study. Each practitioner then searched his or her electronic databases and consecutively extracted 100 patients with a diagnosis of preexisting CHD. The patients were contacted to assess risk factors; after the assessment, the GP reviewed the assessment and ordered relevant diagnostic tests.
Once results were obtained, an in- dividualized patient assessment report was generated automatically using the mdCare system.
Following a review of the reports by the GP, a management plan was developed using a template provided by an mdCare coordinator. The plan was finalized in conjunction with the patient and included a selection of health issues with goals, actions, medications, and allied health refferals as appropriate.
The study focused on risk factors at the time of enrollment. Patients were recruited over a 12-month period between January 2006 and January 2007. The guideline used for cholesterol control incoporated low density lipoprotein (LDL) cholesterol <100 mg/dL and LDL <77 mg/dL, and HDL >38 mg/dL which is the Australian and New Zealand 2005 guideline.
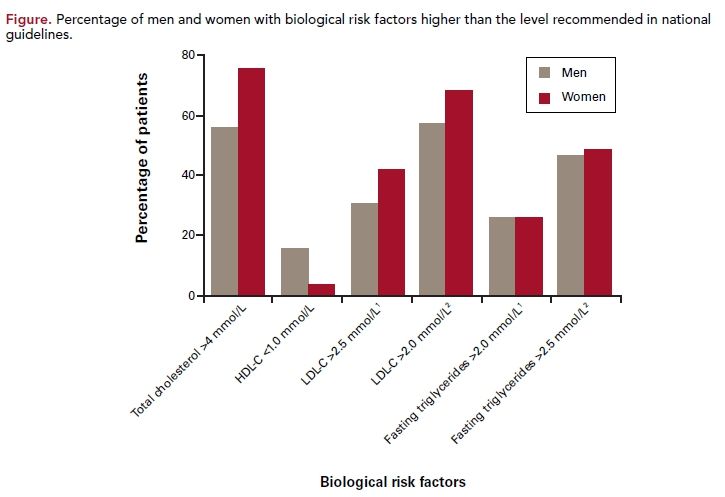
Most GPs participating in this study were more likely to be older, male, and have their practice in a rural setting compared with the total GP population in Australia. Of the 12,509 patients in the study, 7242 were male and 5267 were female. As in other studies, female patients were older; however, unlike in other studies, this study found that men had more cardiovascular comorbidities such as hyperlipidemia, peripheral artery disease, and diabetes, compared with women; women had higher levels of hypertension. More-over, men were more likey to have had a hospital readmission for CHD within the previous 6 months (74% vs 56%, P <0.0001). Men were more likey to smoke, drink alcohol, have a sedentary lifestyle, and eat a diet higher in salt and fat. However, women were more likely to have higher blood pressure than their male counterparts, as well as higher total cholesterol and higher LDL (Figure).
As seen in other studies, Driscoll et al found that women were less likely to be prescribed pharmacotherapy.1,2,4 For example, women were less likely to be taking aspirin (80% vs 71%, P <0.0001), lipid-lowering medications (71% vs 66%, P <0.0001), or antihypertensive medications (62% vs 58%, P <0.0001). The study also found that total cholesterol levels were outside the recommended range in 57% of men and 76% of women with CHD, and among those receiving lipid-lowering medication, a majority of patients were not controlled (53% of men and 72% of women). These patients were selected by the GPs to be enrolled in this study. If the study had been done in a randomly selected patient group, the control rate would be even lower.
On a positive note, both men and women had well-controlled blood pressure. In both groups, the mean systolic and diastolic blood pressure was below 140/80 mm Hg.
References
1. Jneid H, Fonarow GC, Cannon CP, et al. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118(25):2803-2810.
2. Vittinghoff E, Shlipak MG, Varosy PD, et al. Risk factors and secondary preven- tion in women with heart disease: the Heart and Estrogen/progestin Replacement Study. Ann Intern Med. 2003;138(2):81-89.
3. Driscoll A, Beauchamp A, Lyubomirsky G, et al. Suboptimal management of car- diovascular risk factors in coronary heart disease patients in primary care occurs par- ticularly in women. Intern Med J. 2011; doi:10.1111/j.1445-5994.2011.02534.x.
4. Stafford RS. Aspirin use is low among United States outpatients with coronary artery disease. Circulation. 2000;101(10):1097-1101.
5. Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295(2):180-189.
6. MacLaughlin, EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. As- sessing medication adherence in the elder- ly: which tools to use in clinical practice? Drugs Aging. 2005;22(3):231-255.
7. US Department of Health and Human Services Office of Inspector General. Medi- cation regimens: causes of noncompliance. http://oig.hhs.gov/oei/reports/oei-04-89- 89121.pdf. Published June 1990. Accessed November 2, 2011.
COMMENTARY
Women’s Undertreated Cardiovascular Risk Factors
W
hat does this study add to our current knowledge base regarding treatment in our CHD patients? The message is clear: in general, risk factor control for CHD patients leaves much to be desired, whether we live in the United States, Europe, or Australia.5 Another important finding is that regardless of gender, optimal risk factor control remains less than optimal. As in previous studies, Driscoll et al show once again that women are consistently undertreated.1,2,4
Why is there so much clinical inertia? Is it a knowl- edge gap among physicians, lack of compliance by the patients, or some combination of the two that is contrib- uting to lower rates of risk factor control?
Let us first address the role of the physician. As core measure programs in the United States have shown, when physicians and hospitals are audited for core measures such as aspirin use or β-blocker use in myocardial infarction patients, compliance rates improve. Thus, a certain amount of supervision and reminders for physicians are needed to improve the rate of risk factor control. A program in which there is constant feedback may be helpful in outpatient settings as well. Also, a team approach to coordinate care that involves physicians, nurses, and pharmacists can help physicians provide the best care to patients. In an era of aging population and rising costs, such programs are sorely needed.
Clearly there are patient-specific factors that play into medication and treatment compliance. Studies have shown that 55% of elderly patients fail to comply in some way with their medication regimen. In a survey by the American Association of Retired Persons in 2004, 25% of respondents said they had not filled a prescription written by their physician in the past 2 years.6 In a survey by the American Heart Association, 12% of the survey participants said they did not fill their prescription, 12% did not take the medication after it was filled, and 22% take less of the medication than prescribed by their physician. These are startling statistics that should give all clinicians pause.3
Why are patients noncompliant? There are 4 well- known factors responsible for nonadherence to treatment: physiological, behavioral, treatment-related, and factors concerning practitioner/patient interaction.6,7 Physiological factors are patients’ sensory impairment or mobility limitations that prevent them from taking the medication or filling the medication properly. Moreover, patients are less likely to take medication for prevention, whereas they are more likely to comply with symptom- relieving medications. Behavioral factors also play a large role, such as factors involving social isolation and lower socioeconomic status; certain social and health beliefs can also be barriers to compliance. Treatment factors including medication side effects or perceived side effects lead patients to stop taking medications. Poor communication between provider and patient also limits compliance.
Clearly, the issues of management and treatment of patients are complex and require more than just a physician prescribing the correct medications. Some innovative programs have been used to increase best practice patterns, such as a disease-oriented team approach using other medical personnel such as nurses and pharmacists along with physicians. Additionally, increasing our connectivity with our patients via e-mail, mobile phone, or with monetary incentives to take medications have also been used. Instead of blaming physicians, patients, or “the system,” we should focus our energy on how to improve our system so that our patients can actually benefit from medications that have been shown to save lives and prevent morbidity.
About the Author
Leslie Cho, MD, FACC, is director of the Cleveland Clinic’s Women’s Cardiovascular Center. She is also section head, preventive cardiology and rehabilitation in the Robert and Suzanne Tomsich Department of Cardiovascular Medicine at Cleveland Clinic. Dr Cho is board-certified in interventional cardiology, cardiovascular medicine, and internal medicine, and specializes in heart disease in women. She received her MD from the University of Chicago Pritzker School of Medicine. Dr Cho’s residency in internal medicine was at the University of Washington Medical Center, where she received the John Humphrey Award as Most Outstanding Internal Medicine Resident. Her fellowship in cardiology, followed by a fellowship in interventional cardiology and peripheral disease, were at Cleveland Clinic.
