The Cryptococcus Neoformans Effect
A case study published in the Indian Journal of Critical Care Medicine observed the effect of Cryptococcus neoformans on patients with already compromised immune systems.
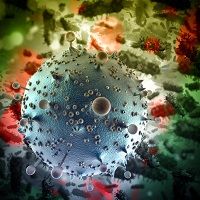
A case study published in the Indian Journal of Critical Care Medicine observed the effect of Cryptococcus neoformans on patients with already compromised immune systems.
The study found that only candidiasis and aspergilossis are more common fungal infections than cryptococcosis. Before citing 2 cases the authors noted that the condition can be particularly dangerous for certain groups of the population.
“Among human immunodeficiency negative (HIV) — negative patients, liver cirrhosis is an important risk factor for cryptococcal disease, with multiple case reports describing this association,” they said. “However, liver disease as a predilection for cryptococcal disease is often under-appreciated, with resultant delay in diagnosis, and poor outcome.”
The first case studied involved a 65-year-old man who was admitted with “progressive jaundice, weakness, and increasing ascites,” over the course of the past month. The diagnosis he received was for chronic hepatitis B-related cirrhosis, with virus-related flare leading to hepatic decompensation.”
Following a series of tests the patient was treated with meropenem but the authors noted his condition worsened before being moved to the intensive care unit. Further testing revealed “encapsulated budding yeast cells, with morphology suggestive of Cryptococcus neoformans.”
After further testing the patient was treated with amphotericin-B (AmBisome 50 Mg/day) as well as cefoperazone-sulbactam. He also underwent ascetic fluid paracentisis in 3-day intervals. The cultures showed C. neoformans continuing to grow and while bacterial cultures were negative, “The urine cultures grew Candida tropicalis that persisted despite catheter change.”
The patient’s condition continued to worsen as he developed lactic acidosis and worsening kidney function with anuria. After his next-of-kin opted to stop further treatments the patient reportedly died within two weeks.
An autopsy of the patient showed “cirrhosis, neutrophilic cholangiolitis, and cellular and canalicular cholestasis.”
The second case involved a 57-year-old man who was admitted to the intensive care unit with hepatitis C virus-related cirrhosis. The patient was complaining of several symptoms including fever, abdominal pain, and increasing ascites.
Similar to the previous patient ascetic fluid samples continued to grow the same fungal species after 2 days. However, after being treated with intravenous fluconazole 200 mg once daily, and Levofloxacin 500 mg once daily for 7 days the patient’s condition improved and he was discharged.
Looking at the 2 cases the authors noted that a diagnosis of fungal peritonitis can be difficult to decipher given some of the “nonspecific.” They added, “However, negative bacterial cultures, prolonged course of infection, recent antibiotic use, and history of previous ascetic fluid sampling may be useful clues.”
As for cryptococcal peritonitis, the authors said, “frequent abdominal paracnetesis with bedside inoculations of fungal culture medium, India ink preparations, and serum and/or ascetic fluid cryptococcal antigen testing by latex agglutination or enzyme immunoassay may establish the diagnosis.”
After discussing other possible diagnoses the authors reported that Cryptococcus organisms were not found in the biopsy of the patient who died, “possibly because we did not use special stains to highlight the fungal elements.”
“Among both immunocompromised and immunocompetent patients, the most common clinical manifestation of cryptococcal infection is meningo-encephalitis,” the authors said. “CSF examination is often not possible due to coexisting coagulopathy in patients with decompensated cirrhosis, as in our patients.”
The authors also noted that the climate in India where the cases were reported also played a role in the development and diagnosis of the conditions.
“The tropical climate of the Indian subcontinent offers a suitable environment for C. neoformans. There is widespread environmental prevalence of Cryptococcus species in India, and many reports of neurological infections in patients with and without HIV infection.”
While that has been a constant concern in India, the authors added, “There are only 2 previous reports of cryptococcal infection in patients with cirrhosis from this country, describing spontaneous cryptococcal peritonitis in 2 patients, and pleural fluid infection in one patient with decomponsated cirrhosis.” Concluding, “It is likely that cryptococcal peritonitis is an under-reported infection among patients with cirrhosis.”
