A Man with Syphilis, Heart Failure, and Buckshot on Radiographs
Left untreated or inadequately treated, syphilis may cause tertiary cardiovascular disease, one form of which is syphilitic aortitis.
James D. Collins, MD
A 55-year-old man presented with several signs and symptoms of progressive congestive heart failure (CHF), including shortness of breath, orthopnea, and paroxysmal nocturnal dyspnea. He also had a diastolic murmur that was discovered approximately 20 years ago during an insurance examination.
The man was diagnosed with syphilis at age 19 and later treated with penicillin at age 30 when the drug became available. Asked about the small metal densities displayed on his plain chest radiographs, the patient admitted he was peppered with buckshot after getting caught with another man’s girlfriend.
The patient’s positive findings included headache, a blood pressure (BP) of 180/40, and cardiac abnormalities. His point of maximum impulse (PMI) was palpable at the seventh intercostal space in the midaxillary line, and a thrill was felt along the left sternal border.
The man had grade 4/6 diastolic decrescendo murmurs that were loudest along the left sternal border at the third intercostal space. A Venereal Disease Laboratory Research (VDRL) test result was reactive for the spirochete, Treponema pallidum.
Radiographic Findings
The patient’s posterior-anterior (PA) chest radiograph (Figure 1) displayed an enlarged left ventricle against the medial margins of the left lateral ribs; left ventricular contour with depression of the left diaphragm; notching of the posterior right fourth and left fifth and sixth ribs; small metal densities over the right lower lung, hypochondrium, and left upper lung; and a lobulated descending aorta.
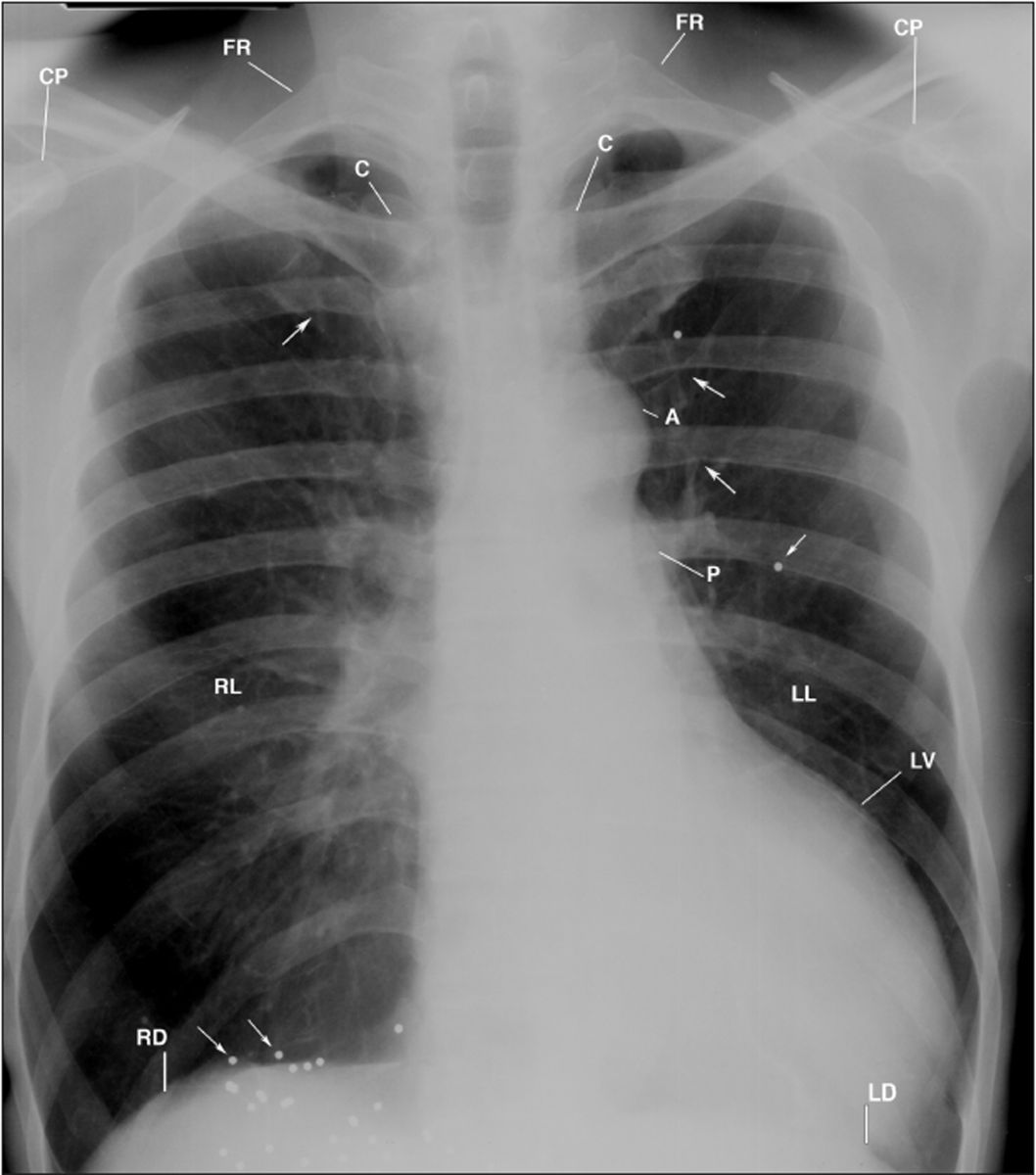
Figure 1
This PA chest radiograph displays hyperexpanded left and right lungs (LL, RL), dilated ascending aorta (A), large left ventricle (LV), metal buckshot (small arrows), notching of the posterior inferior right fourth rib, posterior inferior left fifth and sixth ribs (single long arrows), and cephalization in the lungs and the heart below the left hemidiaphragm (LD). C= clavicle; CP= coracoid process; FR= first rib; P= left pulmonary artery; RD= right hemidiaphragm.
Thin subcutaneous tissues, a narrow thorax, and hyperaeration of the lungs accentuated the near reversal of the patient’s pulmonary vascularity, particularly in the left lung. Small linear densities in the right lateral margins of the left mid-lung reflected lymphatic stasis, or parenchymal scarring.
The lateral chest radiographs (Figure 2-3) displayed dilatation of the ascending aorta; posterior displaced left lower lung bronchi; enlarged rounded left ventricle extending beyond the retrocardiac space and displaced over the lower thoracic vertebrae; metal densities; and tortuosity of the entire thoracic aorta. The narrow thorax accentuated the massive enlargement of the left ventricle.
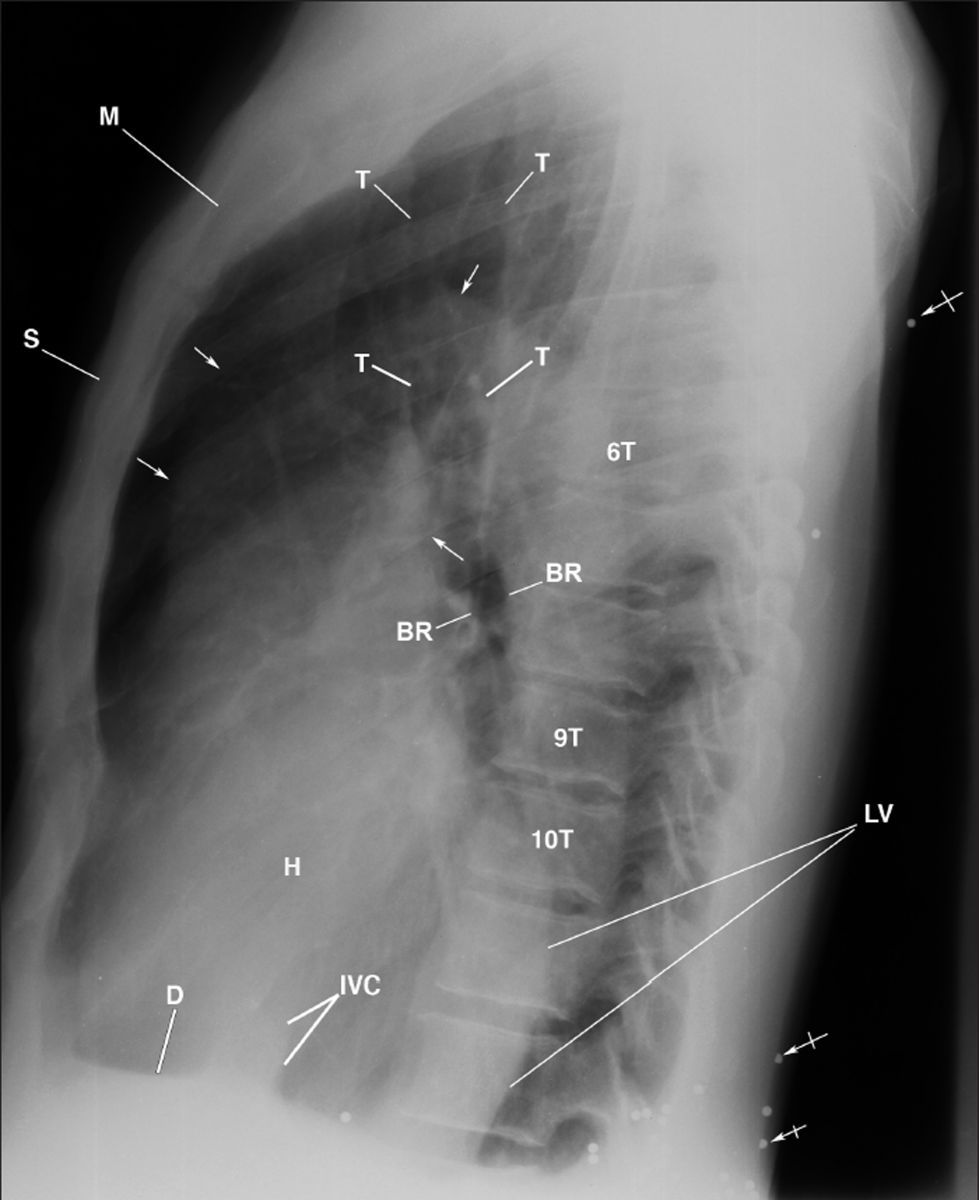
This lateral chest radiograph displays the dilated ascending aorta (arrows), enhanced density of the large left ventricle (LV) extending over the thoracic vertebrae (6T-10T), the heart (H) against the sternum (S), and buckshot (bar arrows) within posterior subcutaneous tissues. Observe the lucency of the posterior displaced left mainstem bronchus (BR) due to the enlarged left ventricle. D= left hemidiaphragm; IVC= inferior vena cava; M= manubrium; T= trachea.
Figure 2
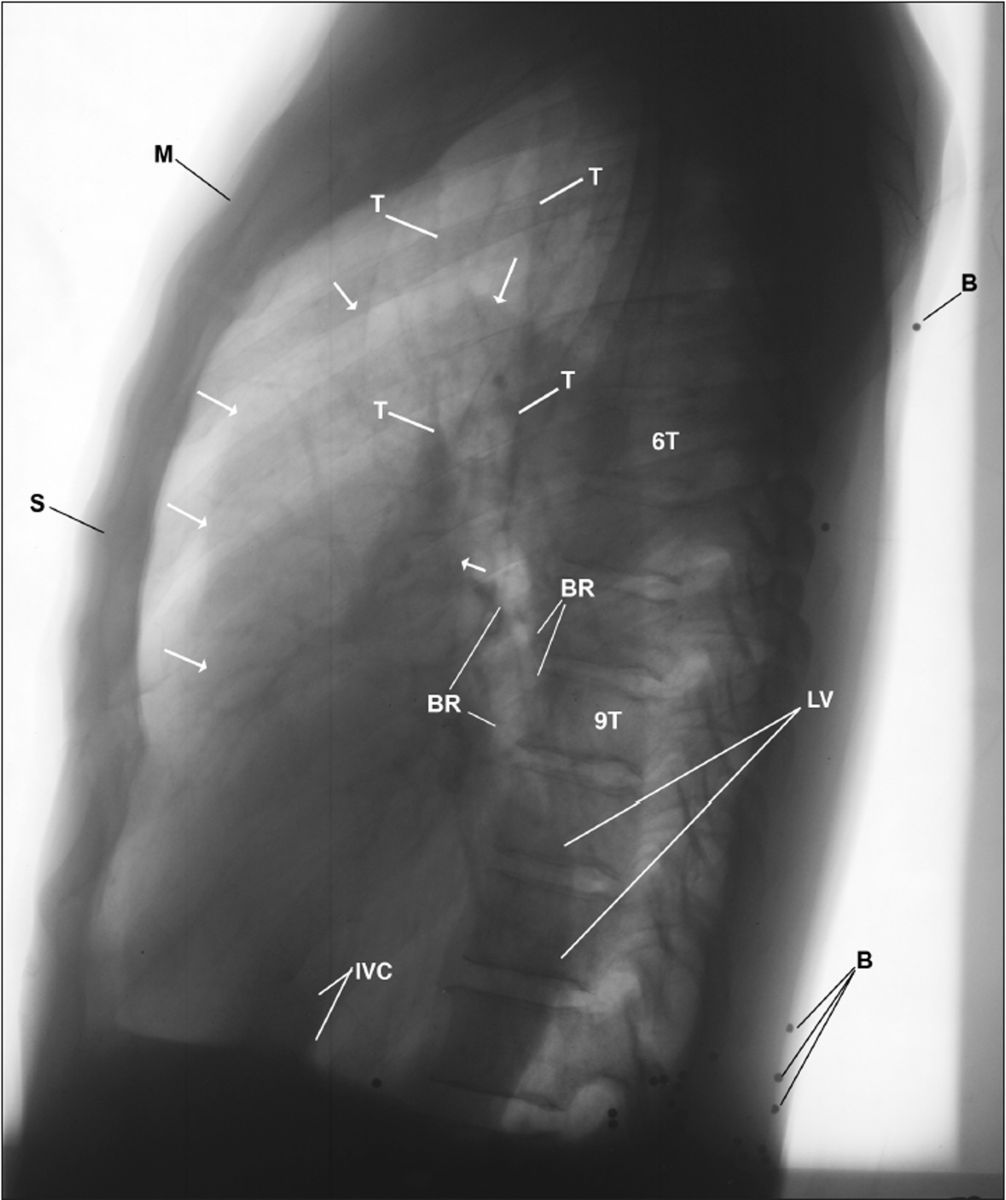
Figure 3 This inverted image of Figure 2 provides a different perspective of the landmark anatomy. Observe the accentuated trabecular pattern of the osseous structures, particularly the end plates of the thoracic vertebrae (6T-9T), margins of the vascular structures, buckshot (B) within the posterior subcutaneous tissues, dilated ascending aorta (arrows), backward displaced bronchi (BR), left ventricle (LV) over the thoracic spine, and the anterior bowed body of the sternum (S).
Diagnosis
Based on those radiographic findings, the man was diagnosed was syphilitic aortitis (SA) with complications from buckshot wounds.
Discussion
Syphilis is transmitted sexually through direct contact with lesions caused by T. pallidum that occur mainly on the external genitalia, vagina, or anus, although they may also emerge on the lips or in the mouth. While syphilis can also be transferred from mother to fetus during pregnancy, it does not spread through contact with toilet seats, doorknobs, swimming pools, hot tubs, bathtubs, shared clothing, or eating utensils.
The incidence of syphilis has declined dramatically since effective antibiotic treatment was first introduced. Nevertheless, syphilis outbreaks continue to occur in the United States, and the infection has been associated with high-risk behaviors, including injection drug use and unsafe sexual behavior. For these reasons, it is unlikely that tertiary syphilis in the form of SA will vanish; if anything, it may be seen more frequently.
Many patients infected with syphilis are asymptomatic for years; however, they remain at risk for late complications if their condition is left untreated. Cardiovascular syphilis typically occurs 15-30 years after the initial syphilis infection and is manifested by the destruction of the media by spirochetes, fragmentation of elastin, and aortic dilatation. The marked dilatation at the base of the aorta eventually leads to aortic insufficiency and the formation of aneurysms.
In this man, a BP of 180/40 reflected AI, and his radiographic features combined with his clinical history of syphilis and reactive VDRL test result made the presumptive diagnosis of SA. Although his presenting headache was not investigated, it may have resulted from impeded venous return and increasing intracranial, intrathoracic, and intra-abdominal pressures.
Take-home Message
Knowledge of the anatomy and pathophysiology of syphilis is important in understanding this case. Left untreated or inadequately treated, syphilis may cause tertiary cardiovascular disease, one form of which is SA that most often affects the ascending portion of the thoracic aorta, as documented by this man’s chest radiographs.
Suggested Reading
1. Dzau VJ, Creager MA. (2005). Diseases of the aorta. Harrison’s Principles of Internal Medicine. (16th ed.). New York: McGraw-Hill.
2. Pugh PJ, Grech ED. Images in clinical medicine. Syphilitic aortitis. N Engl J Med. 2002 Feb 28;346(9):676.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation. Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.