American Academy of Pediatrics Debuts Historic Pediatric Obesity Guidelines
Published in Pediatrics on January 9, the document represents the first comprehensive guideline from the American Academy of Pediatrics in more than a decade and the first ever on the evaluation and management of obesity in those aged 2 years and older.
Sarah Hampl, MD

The American Academy of Pediatrics has released its first comprehensive guidance for evaluation and management of obesity in children and adolescents.
The organization’s first comprehensive guideline in more than a decade, the document, which was released on January 9, provides recommendations related to the role of behavioral interventions, lifestyle treatment, pharmacotherapy, and metabolic and bariatric surgeries in management of obesity in children as young as 2 years of age.
“The medical costs of obesity on children, families and our society as a whole are well-documented and require urgent action,” said Sarah Hampl, MD, professor of Pediatrics at the University of Missouri-Kansas City and chair of the Clinical Practice Guideline Subcommittee on Obesity, in a statement from the American Academy of Pediatrics. “This is a complex issue, but there are multiple ways we can take steps to intervene now and help children and teens build the foundation for a long, healthy life.”
With obesity linked to an increased risk of a multitude of deadly comorbidities, early-life interventions stand to have a significant impact on mitigating this ballooning burden. Citing its associations with short- and long-term health concerns, the American Academy of Pediatrics' first comprehensive guideline for the evaluation and management of obesity were created by a multidisciplinary group of experts in conjunction with primary care providers and a family representative.
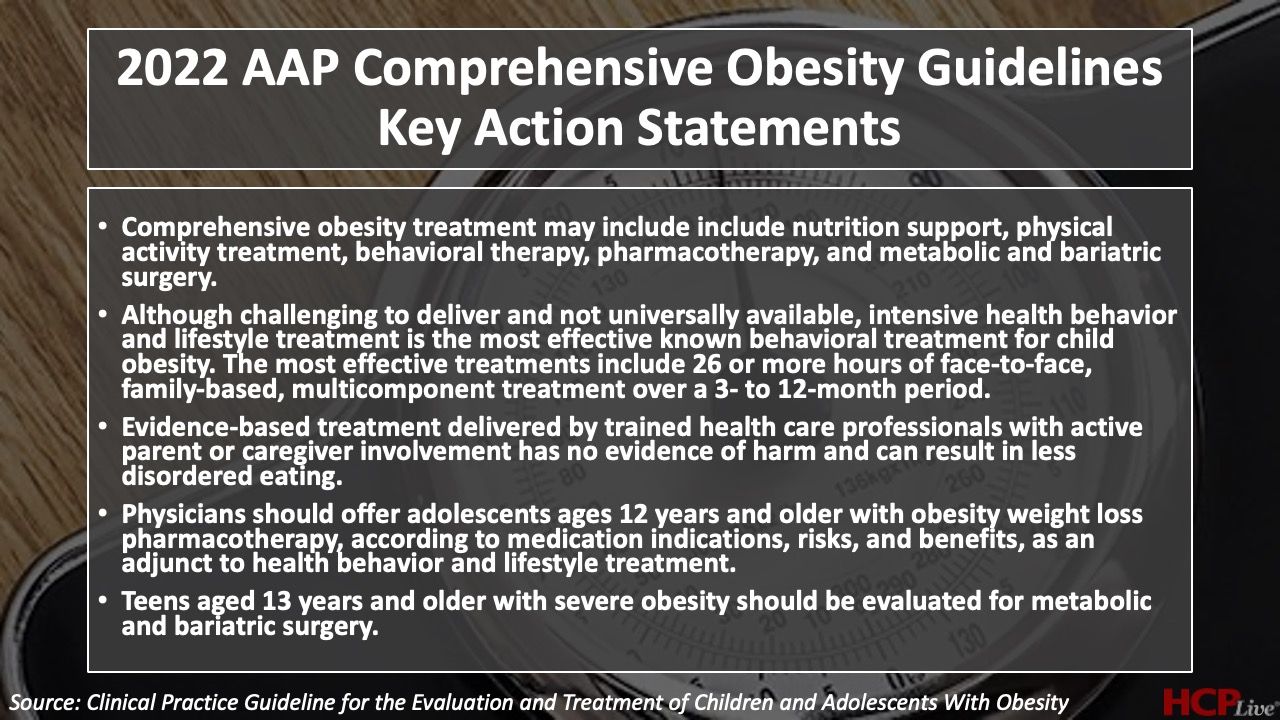
The guidelines were released in conjunction with a pair of technical reports titled “Appraisal of Clinical Care Practices for Child Obesity Treatment. Part I: Interventions,” and “Appraisal of Clinical Care Practices for Child Obesity Treatment. Part II: Comorbidities”. Highlighted within the guideline are the organization’s key action statements, which spotlight a group of 5 specific evidence-based recommendations for evaluating and treating children with overweight and obesity and related health concerns.
“There is no evidence that ‘watchful waiting’ or delayed treatment is appropriate for children with obesity,” said Sandra Hassink, MD, a past president of the American Academy of Pediatrics and vice chair of the Clinical Practice Guideline Subcommittee on Obesity, in the aforementioned statement. “The goal is to help patients make changes in lifestyle, behaviors or environment in a way that is sustainable and involves families in decision-making at every step of the way.”
In addition to addressing clinical factors in the evaluation and management of obesity in this patient population, a portion of the guideline is dedicated to inequities contributing to trends in obesity in childhood. Specific inequities mentioned within the guideline included marketing of unhealthy food, low socioeconomic status, household food insecurity, and structural racism. Notably absent from the guideline are recommendations or discussions surrounding the prevention of obesity in this patient population, which the American Academy of Pediatrics states will be addressed in a forthcoming policy statement.
In the aforementioned statement, the American Academy of Pediatrics called for the strong promotion of supportive payment and public health policies that cover comprehensive obesity prevention, evaluation, and treatment. Additionally, the group brought attention to the need for policy changes that target the presence of structural racism driving alarming and persistent disparities in childhood obesity.
“Research tells us that we need to take a close look at families—where they live, their access to nutritious food, health care and opportunities for physical activity—as well as other factors that are associated with health, quality-of-life outcomes and risks,” Hampl added. “Our kids need the medical support, understanding and resources we can provide within a treatment plan that involves the whole family.”
This guideline, “Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity,” was published in Pediatrics.