Diuretic Use in Black Patients With Uncontrolled Hypertension

Samuel J. Mann, MD
Review
Gerber LM, Mann SJ, McDonald MV, Chiu Y-L, Sridharan S, Feldman PH. Diuretic use in black patients with uncontrolled hypertension. Am J Hypertens. 2013;26(2).
It has been widely shown that diuretics are more effective in lowering blood pressure in black patients than are angiotensin- converting enzyme inhibitors (ACEIs), angiotensin-receptor blockers (ARBs), and ß-blockers. In treating hypertension in blacks, diuretics and calcium channel blockers (CCBs) are the recommended first-step agents.1 Further, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) reported that in blacks, the outcome was better after treatment with diuretics than it was following treatment with ACEIs.2,3 Adding to the good news about diuretics, they are among the most affordable drugs available.
It is therefore surprising that diuretic use has not significantly increased in the period between 2004 and 2008, after the ALLHAT report.4 Also surprising was a recent study reporting that diuretics were prescribed in only 38% of hypertensive blacks.5 In this context, the current study looked at the use of diuretics in a population seemingly ideally suited for diuretic therapy: black patients with uncontrolled hypertension.
Study Details
The study by Gerber and colleagues was conducted in the post-acute care division of a large urban, Medicare/Medicaid-certified home health care organization. Study participants were black, English-speaking, aged 21 to 80 years, with a primary, secondary, or tertiary diagnosis of hypertension (ICD9- CM401, 402, 403, or 404) on admission in the electronic health record. Only those with uncontrolled hypertension, defined by blood pressure readings >140/90 mm Hg (or >130/80 mm Hg for patients with diabetes) at the time of the study recruitment interview, were included. Patients with a diagnosis, by either self-report or ICD codes, for either congestive heart failure or chronic kidney disease, in whom diuretics might be prescribed for reasons other than hypertension, were excluded from the sample.
Data were drawn from an in-home interview, conducted by trained interviewers. Blood pressure measurements were obtained by trained interviewers using a Microlife 3AA1-2 blood pressure device (Microlife USA, Inc, Clearwater, Florida), which uses an oscillometric algorithm validated using the British Hypertension Society criteria. The monitor was programmed to obtain 3 readings and record the average.
The in-home interviewers recorded all the prescribed medications that patients reported taking, identifying all antihypertensive medications. Components of combination pills were recorded as separate drugs, with the sole exception of the combination containing 25 mg of hydrochlorothiazide (HCTZ) with 37.5 mg of triamterene, which was recorded as HCTZ 25 mg only because of the insignificant antihypertensive effect of 37.5 mg of triamterene.
The study included 658 patients, whose mean blood pressure was 155.3/87.4 mm Hg. Although all had uncontrolled hypertension, only 46% were taking a diuretic. The proportion taking diuretics included 32.6% of underweight/normal weight, 43.1% of overweight, and 55.3% of obese participants. The proportion among diabetics and non-diabetics was 46.9% and 43.8%, respectively.
A total of 5.5% of the patients were not on any antihypertensive drugs. Twelve percent of those who were taking just 1 drug were on a diuretic, 43% of those taking 2 drugs were taking a diuretic, 73% of those taking 3 drugs were taking a diuretic, and 90% of those taking ≥4 drugs were taking a diuretic. Viewed another way, among 385 patients with uncontrolled hypertension who were taking 1 or 2 drugs, only 29.6% were taking a diuretic.
Among those whose systolic blood pressure (SBP) was 140 mm Hg to 159 mm Hg, 52.8% were taking a diuretic. Among those with more severe elevation of blood pressure (SBP ≥160 mm Hg), only 44.3% were on a diuretic (P = 0.035). In contrast, ACEI or ARB use was higher in the group with more severe blood pressure elevation (70.8% vs 61.4%, P = 0.013).
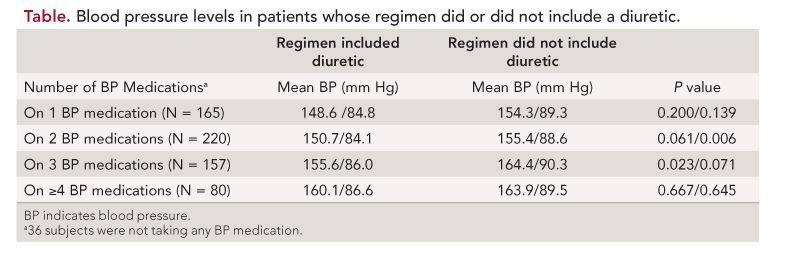
Among patients on a single drug, blood pressure was lower among those who were taking a diuretic than those who were not.
Similarly, among patients who were on 2, 3, and ≥4 drug regimens, blood pressure was lower among those whose regimen included a diuretic than among those whose regimen did not. Thus, regardless of the number of drugs taken, blood pressure was consistently higher if a diuretic was not included in the regimen.
Finally, the authors note that among those who were on a diuretic, 67.3% were taking HCTZ, and the dose in 93.1% of those patients was ≤25 mg/d. Only 6.9% were taking a stronger regimen, such as a higher dose or a combination with a potassium- sparing agent. Thus, even when a diuretic was prescribed, a regimen stronger than 25 mg of HCTZ was not commonly prescribed.
References
1. Flack JM, Sica DA, Bakris G, et al. International Society on Hypertension in Blacks: management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks Consensus statement. Hypertension. 2010;56:780-800.
2. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid- Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981- 2997.
3. Einhorn PT, Davis BR, Wright JT Jr, Rahman M, Whelton PK, Pressel SL; ALLHAT Cooperative Research Group. ALLHAT: still providing correct answers after 7 years. Curr Opin Cardiol. 2010;25:355-365.
4. Stafford RS, Bartholomew LK, Cushman WC, et al; ALLHAT Collaborative Research Group. Impact of the ALLHAT/JNC7 Dissemination Project on thiazide-type diuretic use. Arch Intern Med. 2010;170:851-858.
5. Odigie-Okon E, Zarich S, Okon E, Dufresne A. Antihypertensive therapy in African Americans: findings from an inner-city ambulatory clinic. J Clin Hypertens. 2010;12:187- 192.
6. Kiowski W, Buhler FR, Fadayoni R. Age, race, blood pressure and renin predictors for antihypertensive treatment with calcium antagonists. Am J Cardiol. 1986;56:81H-8H.
7. Jamerson K, Weber MA, Bakris GL, et al. ACCOMPLISH trial investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359:2417-2428.
8. Setaro JF, Black HR. Refractory hypertension. N Engl J Med. 1992;32:543-547.
9. Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003;16:925-930.
10. Khosla N, Chua DY, Elliott WJ, et al. Are chlorthalidone and hydrochlorothiazide equivalent blood pressure-lowering medications? J Clin Hypertens. 2005;7:354-356.
11. Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43:4-9.
12. Messerli FH, Makani H, Benjo A, Romero J, Alviar C, Bangalore S. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring: a meta-analysis of randomized trials. J Am Coll Cardiol. 2011;57:590-600.
Commentary Documenting Underuse of Diuretics in a Population That Needs Them
Diuretics have been consistently shown to be effective in lowering blood pressure and preventing cardiovascular events in many populations, and particularly in black populations. Previous studies have documented their underuse in black patients, even in the aftermath of the ALLHAT study. This study goes further in documenting their underuse, even in black patients with uncontrolled hypertension, despite their effectiveness and low cost.
One could argue that some of the patients, despite an elevated reading recorded at a single visit, might not truly have had uncontrolled hypertension. However, the study found that diuretics were being taken in a lower proportion of patients whose SBP exceeded 160 mm Hg than among those whose SBP was 140 mm Hg to 159 mm Hg. The lower proportion of use in the subgroup with the more severe blood pressure elevation strongly suggests that nonuse of diuretics is contributory to the higher readings in this subgroup.
The obvious question that arises is why physicians are not prescribing diuretics in more of these patients. Managed care considerations would actually favor the increased use of inexpensive diuretics such as HCTZ. Yet although the ALLHAT study reported that diuretics were at least as effective as other drug classes in controlling hypertension and preventing cardiovascular events, there was little subsequent increase in their use in the years following publication of that study.4
One factor could be concern about the adverse metabolic effects of diuretics, particularly at higher dosage, effects that do not accompany the use of CCBs, ACEIs, and ARBs. Concern over glucose homeostasis in diabetics can be suggested, although in this study, the use of diuretics was higher in diabetics than in non-diabetics. Prior intolerance to diuretics is also an unlikely explanation, as the rate of discontinuation of diuretics is not high.
Further, adverse effects such as hyperglycemia, hypokalemia, and hypomagnesemia are minimized by the commonly used low doses of thiazide diuretics. And the alternative of combining a thiazide diuretic with a potassium-sparing agent can reduce the likelihood of adverse metabolic effects when a stronger regimen is needed. In patients with a history of adverse reaction or contraindication to a thiazide diuretic, physicians can still safely prescribe a diuretic, by prescribing a loop and/or potassium- sparing diuretic instead of a thiazide diuretic, for example, a loop diuretic in patients with a history of thiazide-induced hyponatremia, or a potassium- sparing diuretic in patients with thiazide-induced hypokalemia.
One could also argue that among black patients a CCB is a valid alternative to a diuretic, given their effectiveness in lowering blood pressure in volume-mediated hypertension, and the superiority, in terms of cardiovascular events, of an ACEI/CCB combination over an ACEI/diuretic combination, as reported in the ACCOMPLISH trial.6,7 However, several factors argue against this explanation. First, the data in this study were obtained prior to the reporting of the ACCOMPLISH trial. Second, even allowing for the use of a CCB as an acceptable alternative to a diuretic, 31.5% of study participants were on neither a diuretic nor a CCB. Further, among those who were on a CCB and not on a diuretic, given their uncontrolled hypertension, particularly if they were taking 3 or more drugs, there is consensus that a diuretic should have been added or substituted.
Another widespread problem with diuretic use that was superficially addressed in this study is the issue of diuretic dose. Strengthening of the diuretic regimen has been shown to bring hypertension under control in about half the cases of resistant hypertension.8,9 Also, it is often forgotten that in ALLHAT, the diuretic used was 25 mg chlorthalidone, not HCTZ. Twenty-five mg of chlorthalidone is equivalent to 37.5 to 50 mg of HCTZ.10,11
In this study, of the 67% who were taking HCTZ, 93% were taking a daily dose of 25 mg or less, despite the persistence of elevated blood pressure readings. Increasing the dose, or substituting chlorthalidone, or adding a potassium-sparing agent, could be expected to lower the blood pressure of many of these patients. Consistent with this, in a recent meta-analysis, Messerli reported that 25 mg HCTZ lowered ambulatory systolic blood pressure by only 7.6 mm Hg, in contrast to the approximately 12-mm Hg lowering observed with the use of 50 mg HCTZ, or the usual dosage of ARBs, ACEIs, and CCBs.12 Thus, in many of the patients in this study who were taking a diuretic and had uncontrolled hypertension, the strength of the diuretic regimen was too low. The clear conclusion in this study population is that diuretics were both underused and underdosed.
In strengthening the diuretic regimen, the 3 main alternatives are increasing the dose of HCTZ, switching to chlorthalidone, or adding a potassium-sparing diuretic to the HCTZ. Since the use of chlorthalidone 25 mg or HCTZ 50 mg raises legitimate concern about adverse metabolic effects, particularly hypokalemia, it is understandable that many physicians are reluctant to use these effective doses. In this context, the option of combining 25 mg or more of HCTZ with a potassium- sparing diuretic is an attractive but underused alternative in treating uncontrolled hypertension. Unfortunately, outcome studies have focused mostly on chlorthalidone rather than on diuretic combinations that include a potassiumsparing agent. Nevertheless, their favorable metabolic profile supports the likelihood of an outcome that would not be inferior to the proven benefit of chlorthalidone.
In conclusion, this study provides further documentation of the underuse of diuretics in black hypertensive populations, and, as shown here, even among black patients with uncontrolled hypertension. Although many drug classes provide very reasonable and metabolically neutral alternatives to diuretics as first-step drugs, and although a diuretic is not the right drug for everyone, their low rate of usage in a black population with uncontrolled hypertension is simply wrong, and hard to explain. More attention needs to be directed to this very correctable error in hypertension management.
About the Author
Samuel J. Mann, MD, is Professor of Clinical Medicine, Hypertension Division, at NewYork-Presbyterian Hospital, Weill/Cornell Medical School, in New York City. Dr. Mann is the author of many scientific articles, book chapters, and 2 books, the most recent of which, Hypertension and You; Old Drugs, New Drugs, and the Right Drugs for Your High Blood Pressure, was published in 2012. His focus is on improving the management of resistant hypertension by selection of medications that target the mechanism driving an individual’s hypertension.
