Macrolide Antibiotics Frequently Prescribed for Inappropriate Indications
In an effort to identify when and where to target interventions for reducing inappropriate antibiotic prescribing and related bacterial resistance, a new study has described the trends and seasonal variations in antibiotic prescription rates throughout primary care settings.

In an effort to identify when and where to target interventions for reducing inappropriate antibiotic prescribing and related bacterial resistance, a new study published in Antimicrobial Agents and Chemotherapy has described the trends and seasonal variations in antibiotic prescription rates throughout primary care settings.
For their retrospective, cross-sectional analysis, Katie J. Suda, PharmD, Associate Professor of Preventive Medicine in the Department of Clinical Pharmacy at the University of Tennessee Health Science Center in Memphis, and colleagues observed the dispense rate of systemic antibiotic prescriptions in US outpatient settings between 2006 and 2010.
Over that 5-year period, the researchers discovered more than 1.34 billion antibiotic prescriptions were dispensed to patients. Although the annual number of prescriptions remained constant between 2006 and 2010, the total prescribing rate decreased by 2.8% over that time period. In fact, “the (prescribing) rate decreased annually with the exception of 2009, where a 0.4% increase was observed relative to 2008,” which the authors attributed to the H1N1 influenza pandemic.
Though penicillin and cephalosporin were among the most commonly prescribed antibiotic classes throughout the 5-year study period, Suda and her colleagues saw substantial declines in the number of outpatient prescriptions for those medications. However, the prescribing rate of the similarly prevalent macrolide antibiotic class increased by 6.1% between 2006 and 2010 — a trend that “would not have been statistically significant from a random sample, (but) remains clinically significant due to the completeness of the data set,” the investigators explained.
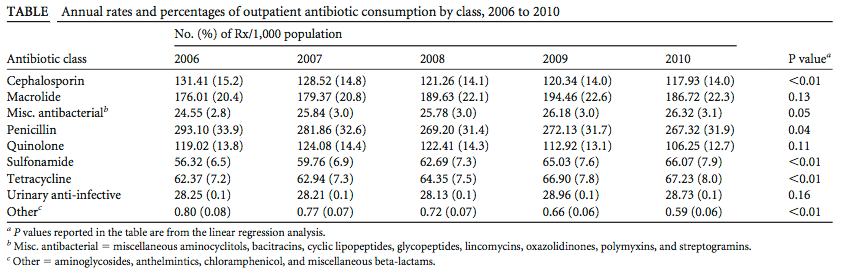
Breaking down the antibiotic prescription data by winter and summer months, the investigators noted an average of 24.5% more prescriptions were dispensed between October and March than between April and September. Yet, that seasonality was consistently dependent on antibiotic class, since it was driven by a 75% increase in penicillin prescriptions and an even more alarming 100% spike in macrolide prescriptions during the winter months.
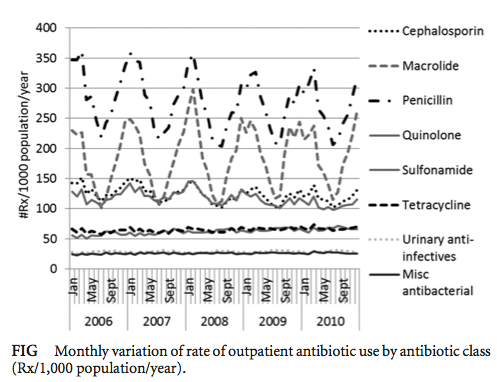
“Inappropriate prescribing of macrolides for infections predominately of viral origin has been previously reported, and it is likely that the fluctuations in the macrolide class in our results represent similar inappropriate indications,” the authors wrote. “Increasingly judicious prescribing of this class is important because outpatient prescriptions for macrolides — the majority for azithromycin — have been associated with bacterial resistance.”
Nonetheless, Suda and her colleagues stressed that the prescription rates of most antibiotic classes decreased over the 5-year study period and were lowest in 2010, which they credited to “patient education, changes in provider behavior, decreases in outpatient visits for acute respiratory infections, and increases in vaccine administration rates.”
“Prescribing of antibiotics is a complex process and is driven by physician attitudes, patient signs and symptoms, and time pressure,” the researchers recognized. “Understanding how antibiotic prescribing varies throughout the year will be useful for designing an optimal intervention strategy to reduce inappropriate antibiotic use, (while) additional years of data will determine if antibiotic consumption continues to decrease.”
