Missed Cervical Ribs Alter Pain Management in Thoracic Outlet Syndrome
A radiograph to detect the presence of a cervical rib should be mandatory prior to thoracic outlet syndrome surgery as a baseline study.
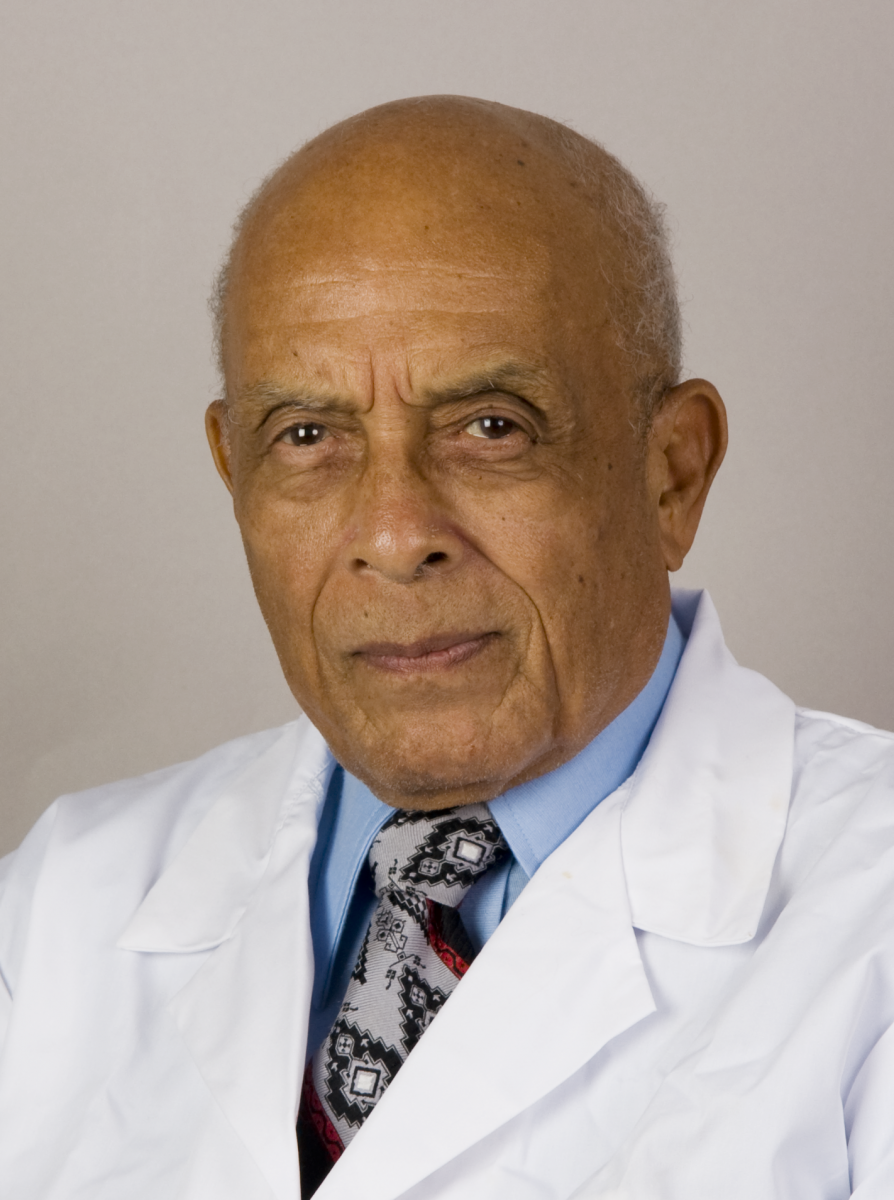
James D. Collins, MD
This 47-year-old, right-handed female physical therapist was referred by a neurologist for bilateral magnetic resonance imaging (MRI) of her brachial plexus. The referring neurologist indicated the patient developed tingling, numbness, and pain in her right arm with right occipital headache following a whiplash injury she sustained on a roller coaster. Thereafter, she reportedly underwent transaxillary resection of her right first rib for right thoracic outlet syndrome (TOS).
After the surgery, the patient suffered persistent pain in her right shoulder and hand, and then 4 months later, she underwent right supraclavicular anterior scalene and middle scalenectomy. Although she received multiple treatments — including Botox injections, physical therapy, and myofascial release of the intercostal muscles — she continued to experience pain and numbness in her right arm that interfered with her work.
One-and-a-half years later, the patient underwent right pectoralis minor tenotomy and neurolysis of the right brachial plexus, but again without relief. Subsequently, the following chest radiograph and bilateral MRI, magnetic resonance angiography (MRA), and magnetic resonance veinography (MRV) of the brachial plexus were obtained.
Radiographic Findings
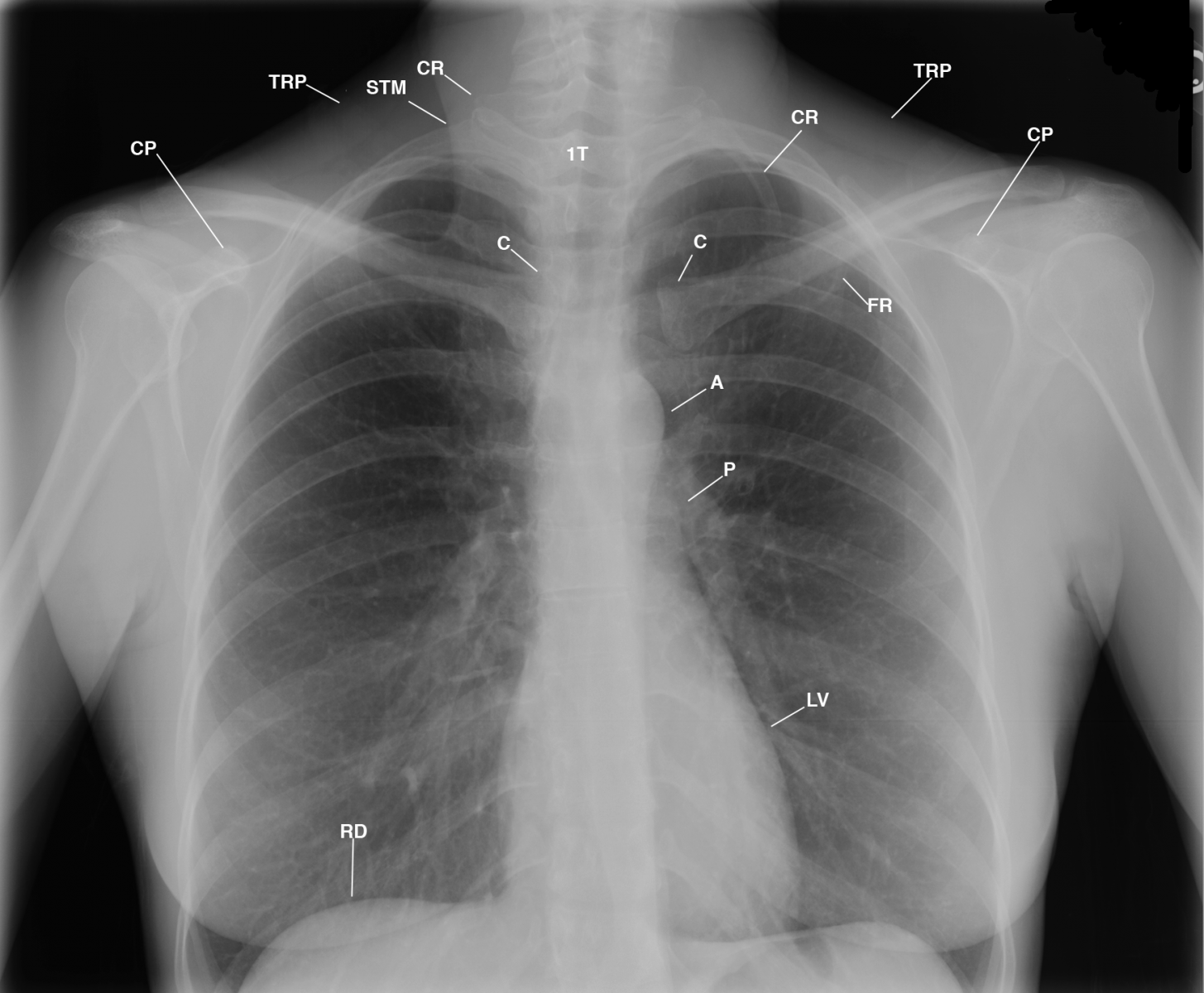
Figure 1
This posterior-anterior (PA) chest radiograph displays sharp margination of the right sternocleidomastoid muscle (STM) atrophy of the right trapezius muscle (TRP) as compared to the left; increased lucency over the apex of the right lung; mild left concave cervicothoracic spine scoliosis, C5-T6 (not labeled); left cervical (CR) and first rib (FR) synchondrosis as the left clavicle crosses over the posterior third intercostal space; resected right cervical rib (CR); residual right costochondral junction of the first rib inferior to the head of the clavicle (C); intact right first rib as it attaches to the manubrium (not labeled); anterior rotated heads of the clavicles, with the right lower than the left; drooping right shoulder as compared to the elevated left shoulder; and normal cardiomediastinal structures and lungs. Observe the decreased soft tissues of the right axilla as compared to the left axilla. A= aorta; CP= coracoid process; LV= left ventricle.
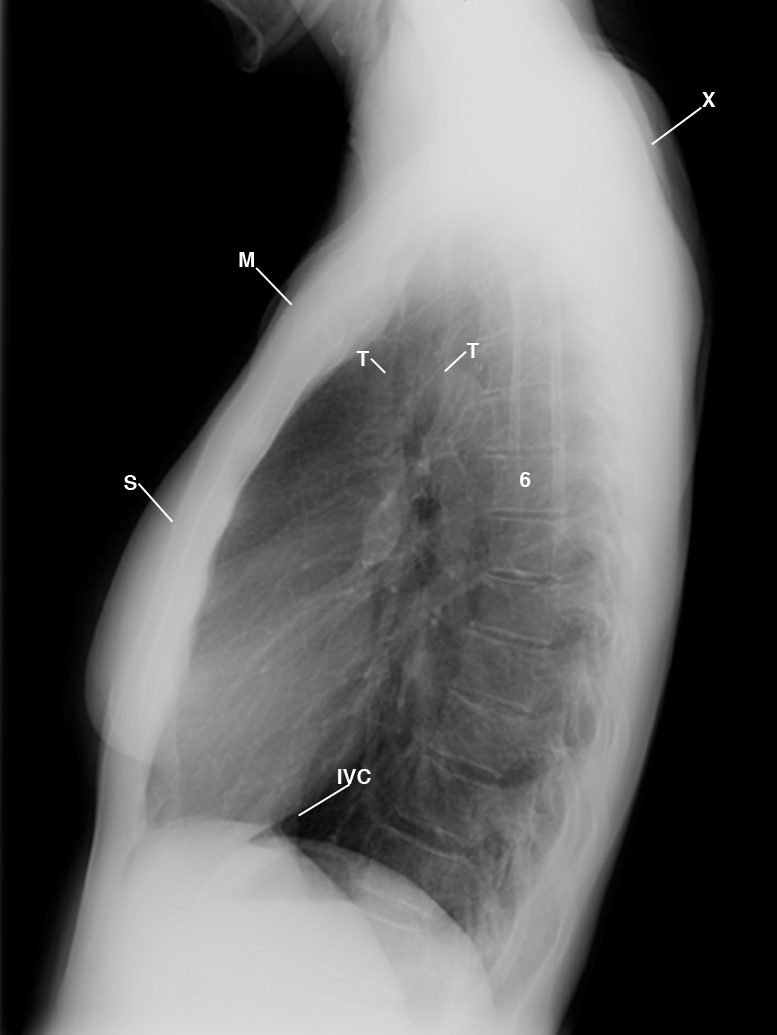
This lateral chest radiograph cross-references the PA chest radiograph to display the thin subcutaneous tissues; fused sternomanubrial joint; backward displaced manubrium (M) placing the heads of the clavicles in close proximity to the increased slope of the first ribs; mild degenerative changes involving the upper anterior margins of the thoracic spine (6); rounding of the shoulders (X); and normal lungs and cardiomediastinal structures. IVC= inferior vena cava; S= sternum; T= trachea.
Figure 2
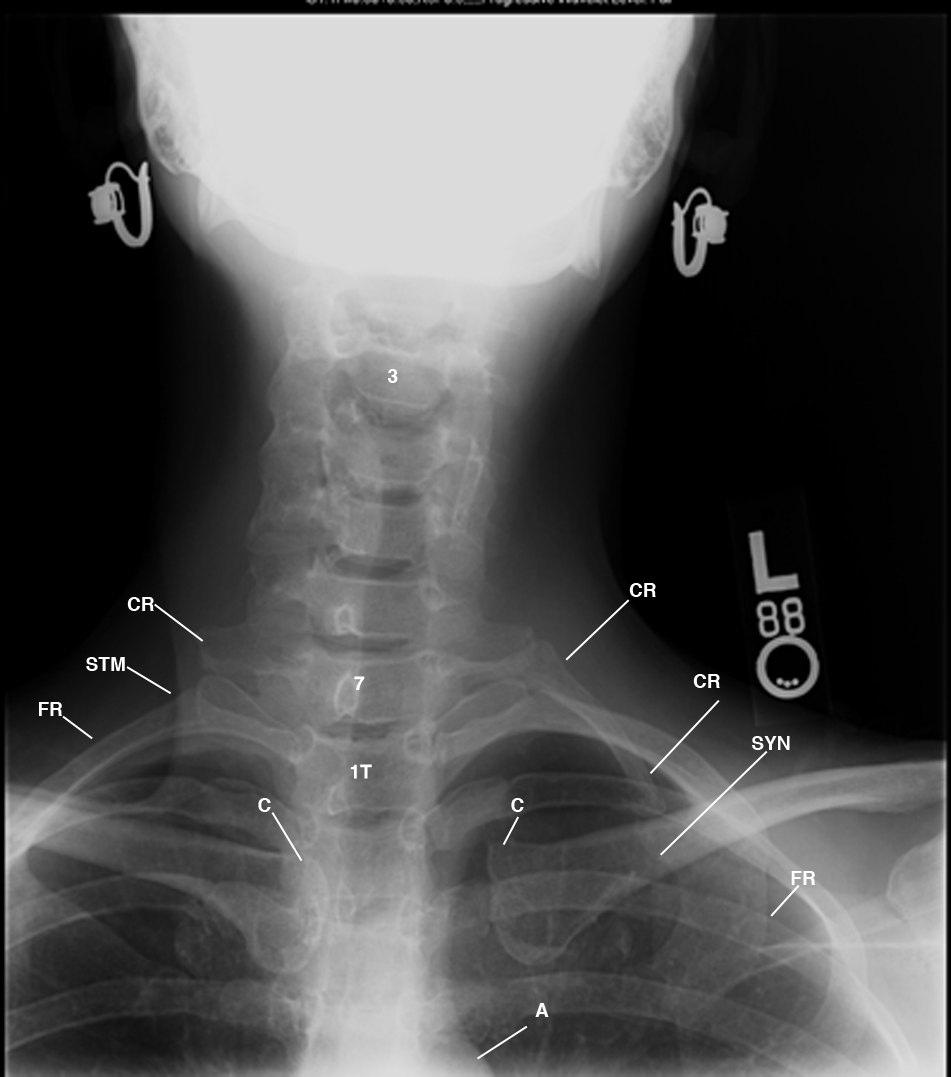
Figure 3 This AP cervicothoracic spine radiograph displays the patient leaning left (L); mild concave curvature of the cervicothoracic spine, C3-T3; synchondrosis deformity (SYN) of the left first (FR) and cervical ribs (CR); and the resected site of the right cervical rib with minimal residual tissue over the apex of the right lung. First thoracic vertebra= 1T;
3, 7= cervical vertebrae

Figure 4 This 3D coronal image displays thin subcutaneous tissues accentuating the narrow chest with the forward dropping right shoulder as compared to the elevated left shoulder; resected right middle scalene muscle (not displayed) as compared to the left; patient leaning to the right; concave depressed right axillary artery (not displayed) with binding nerves and right axillary vein (AXV) reflecting costoclavicular compression on the right first rib (FR); gray proton dense dilated lymphatics (not labeled) converging at the junction of the left thoracic duct (not labeled) and the left internal jugular vein and subclavian veins (not labeled). BR= brachiocephalic trunk; BRV= brachiocephalic vein; C= clavicle; CV= cephalic vein; XJ= external jugular vein; E= esophagus; SA= subclavian artery; SUB= subclavius muscle.
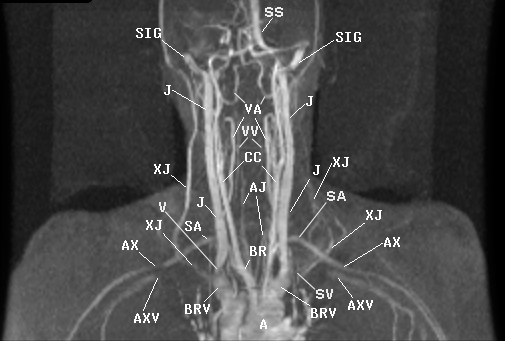
Figure 5 This 3D reconstructed coronal image confirms the T1 weighted images. It displays the backward displaced aorta (A) and pulmonary artery (P) as the great vessels ascend into the neck. The patient leans to the right, elevating the left shoulder (not labeled). The backward displaced manubrium and body of the sternum (not displayed) splay apart the right and left brachiocephalic veins (BRV), shifting the mediastinal contents to the left of midline accentuating the mediastinal shift of the great vessels, including the right internal jugular (J) compressed at the inferior bicuspid valve (V) and subclavian vein (SV), as well as the BRV, reflecting costoclavicular compression of the SV. Observe the cone shaped compressed inferior bicuspid valve (V) within the right internal jugular, reflecting the fibrosis and scarring described above. CC= common carotid artery; J= jugular vein; SIG= sigmoid sinus; TCV= transverse cervical vein; AX= axillary artery; SS= sagittal sinus; VA= vertebral artery; VV= vertebral vein.
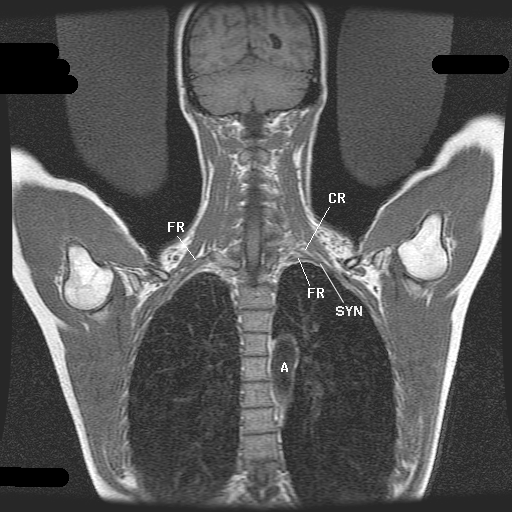
Figure 6 This coronal bilateral abduction external rotation
(AER)
of the upper extremities sequence displays the posterior inferior rotation of the clavicles with the subclavius muscle and lymphatics with the posterior anterior medial rotation of the coracoid processes with attached muscles compressing the draining veins within the neck, supraclavicular fossae with lymphatics and the subclavian arteries and axillary arteries with binding nerve roots, with the right greater than left (not labeled). Observe the right clavicle (not labeled) with the subclavius muscle compressing the soft tissues on the gray proton dense fibrosis and scarring which marginates the resected right scalene triangle on the first rib and low right shoulder (not labeled), reflecting greater laxity of the sling/erector muscles on the right as compared to the elevated left.
Diagnosis
This patient has TOS with recalcitrant symptoms stemming from the surgeon’s failure to remove the right first thoracic rib at the time of the first surgery. Although the surgeon thought he had excised the first thoracic rib, he failed to recognize that the patient had a cervical rib, which resulted in the removal of the incorrect rib.
Discussion
Cervical ribs develop as a result of the elongation of the transverse process of the seventh cervical vertebra (C7).1 They may have an epiphyseal plate or form synchondrosis deformities with the first rib. Although cervical ribs and synchondrosis deformities of a cervical or first rib are typically displayed on a PA chest radiograph, they are often overlooked.2
Laxity of the sling and/or erector muscles of the shoulders causes the C7 and third thoracic vertebra (T3) to shift forward, contributing to kyphosis of the thoracic spine and rounding of the shoulders. In such patients, the cervical rib and synchondrosis of the cervical rib and first ribs cause costoclavicular compression of the adjacent neurovascular bundle — or compression of the second division of the subclavian artery with binding nerve trunks and compression of the bicuspid valves within the subclavian and internal jugular veins — which triggers neurological symptoms such as pain; upper extremity numbness and tingling; weakness of the intrinsic hand muscles; temperature and color changes; visual blurring; headache; neck, hip, groin, and low back pain; and radicular pain in the legs and feet.
MRI, MRA, and MRV display abnormalities that alter fascial planes and result in costoclavicular compression of the bicuspid valves within the lymphatics and draining veins of the neck, supraclavicular fossae, and subclavian and axillary arteries with binding nerves.3 Monitored multiplanar images with abduction external rotation (AER) and 2D time-of-flight (TOF) MRA and MRV without contrast cross-references costoclavicular compression of the brachial plexus on T1-weighted images.
Take-home Message
The purpose of this case is not to highlight MRI as a diagnostic tool, but emphasize the necessity of landmark anatomy in making an accurate diagnosis. In this patient, only the right cervical rib was resected and the right first rib was left behind because a preoperative chest radiograph was not obtained. A radiograph to detect the presence of a cervical rib should be mandatory prior to TOS surgery as a baseline study, and it should be imaged above the fifth cervical vertebra to ensure the display of cervical rib anomalies. You only see what you know.4-5
References
1. Woodburne RT, Burkel WE. (1988.) Essentials of Human Anatomy. (8th ed.). New York: Oxford University Press.
2. Collins JD, Saxton EH, Miller TQ, AHN SS, Carnes A. Synchondrosis of cervical and first ribs causes costoclavicular compression and Paget-Schroetters syndrome: MRI/MRA/MRV. J Natl Med Assoc. 97:885.
3. Collins JD, Saxton EH, Miller TQ, AHN SS, Carnes A. Scalenectomy and incomplete first rib resection fail to relief costoclavicular compression in thoracic outlet syndrome in migraine patients. J Natl Med Assoc. 97:884.
4. Collins JD, Saxton E, Miller TQ, Ahn S, Gelabert H, Carnes A. (2003). Scheuermann’s disease as a model displaying the mechanism of venous obstruction in thoracic outlet syndrome and migraine patients: MRI and MRA. J Natl Med Assoc. 2003;4:298-306.
5.Collins JD, Shaver ML, Disher AC, Miller TQ. (1998). Bilateral MRI of the brachial plexus and peripheral nerve imaging: technique and three-dimensional color, peripheral nerve imaging. Management of Peripheral Nerve Problems. (2nd ed.). Philadelphia: W.B. Sanders.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation. Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.
