Publication
Article
An Exciting ECG...A Little early?
Author(s):
A 36-year-old man presents to his primary care physician's office for follow-up after being told he had an abnormal ECG at a health fair he attended. He has no complaints. He is sedentary and does not participate in any exercise or athletic activity.
A 36-year-old man presents to his primary care physician’s office for follow-up after being told he had an abnormal ECG at a health fair he attended. He has no complaints. He is sedentary and does not participate in any exercise or athletic activity. He has never had chest discomfort, shortness of breath, syncope, palpitations or other relevant cardiac symptoms. He comes with an ECG in hand, which is shown below.
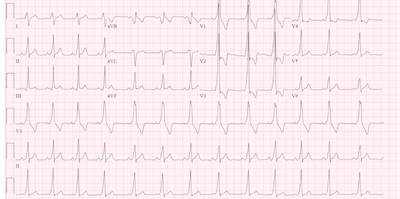
The ECG above shows a wide complex regular rhythm. There is a P wave before every QRS and a QRS for every P wave suggesting sinus rhythm, but the PR interval is very short with the QRS initiating at the end of the P wave in V2-V5. The QRS starts with a slow initial deflection, a relatively fast terminal portion followed by an abnormal ST and T wave segment. These findings are most consistent with a Wolff-Parkinson-White pattern on ECG
The patient has asymptomatic WPW Syndrome, or more appropriately, described as WPW pattern on ECG. WPW pattern is related to an accessory pathway that leads to pre-excitation of the ventricle through a conduction pathway other than the AV node. Because conduction also progresses through the AV node, the pattern typically has a narrow terminal half of the QRS.
Pre-excitation is associated with supraventricular tachycardias (SVT) and sudden cardiac death (SCD). When antegrade conduction through an accessory pathway is preserved at high heart rates, the results can be catastrophic. Atrial fibrillation or flutter can result in hemodynamic instability, particularly if given nodal blocking agents like adenosine or verapamil. Once the node is blocked, the ventricle can be directly stimulated via the accessory pathway, potentially causing ventricular fibrillation. Patients with an accessory pathway and an SVT may need urgent electrical cardioversion, or can be converted pharmacologically with a class I antiarrhythmic like procainamide.
If a pre-excitation pathway is found incidentally in an asymptomatic patient, no treatment may be required. To determine if there is an increased risk of sudden cardiac death, there are noninvasive and invasive assessments that can be performed. If an accessory pathway is seen intermittently on an ECG alternating with a normal PR interval, the risk of SCD may be lower.
Further testing with a holter monitor to look for intermittent pre-excitation can be helpful. Exercise testing can be reassuring if pre-excitation is lost at higher heart rates, suggesting that the accessory pathway cannot conduct fast enough to be a concern during a period of SVT.
However, referral to an electrophysiologist is highly recommended as there are a number of characteristics in the ECG that can impact the overall risk assessment. Occasionally there may be multiple accessory pathways or the pre-excitation pathway may be hidden on surface ECG.
In the end, the only definitive way to be certain of an accessory pathway’s characteristics and propensity for rapid conduction is performing an invasive electrophysiology study. With the increase of ECG’s performed for screening of athletes, WPW pattern is seen more frequently and the noninvasive testing may be used to see who is most appropriate for invasive testing and/or definitive treatment with catheter ablation techniques.
Our patient was referred to an electrophysiologist who performed a stress ECG. At a HR of 110 bpm, the patient lost the delta wave and the QRS narrowed to 88 ms.
A holter monitor showed intermittent loss of the pre-excitation pathway with normal ECG pattern at high heart rates. The supplementary testing suggested the patient was at low risk for arrhythmias that might lead to SCD and an invasive study was deferred.
The four characteristics of an ECG that are highly suggestive of the presence of a pre-excitation pathway include the following:
1.A short PR interval: less than 120 ms in adults and less than 90 ms in children
2.Presence of a Delta Wave: slurred initial upstroke of the QRS that can either start in the P wave or immediately following the P wave.
3.Prolonged QRS: greater than 120 ms in adults and greater than 90 ms in children
4.Secondary ST and T wave changes: typically ST and T wave deflected opposite the delta wave and QRS deflection