Publication
Article
Meeting Report: 23rd Annual Echo Hawaii
23rd Annual Echo Hawaii
Kohala Coast, Big Island, HI
In this issue, Cardiology Review summarizes 6 studies presented at the 23rd Annual Echo Hawaii conference, held January 21-25, 2013, at Kohala Coast, Big Island, HI. The Echo Hawaii conference presents the latest information on established and emerging cardiovascular ultrasound technologies, with a focus on how state-of-the-art technologies can be effectively applied in the clinical setting. The meeting is jointly sponsored by the American Society of Echocardiology (ACE) and the ACE Foundation.
Aortic Knob Calcification on Chest X-ray Predicts Atheroma of Distal Aortic Arch on TEE
Kyung Won Yun, MD, of the Pusan National University Yangsan Hospital, Yangsan, Republic of Korea, presented data showing a correlation between aortic knob calcification (AKC) on chest x-ray and atheroma of the distal aortic arch detected by transesophageal echocardiography (TEE). The study was the first to show the correlation, and suggests that chest x-ray is a useful screening method to provide important clinical information about aortic atheroma.
From January to December 2011, 410 patients who were to undergo TEE at the cardiovascular center at Pusan National University Yangsan Hospital were selected for possible inclusion in the study. After excluding patients who did not undergo chest x-ray or who had an unknown family history or lipid profile, 322 consecutive patients (197 male, 125 female; mean age, 62.2) were included in the final study.
Atheroma thickness was measured in the distal aortic arch and the proximal descending thoracic aorta. Atheroma thickness was divided into <5 mm and ≥5 mm. Atheroma was classified as simple (presence of calcification only) and complex (presence of calcification with ulceration or mobile plaque or hypoechoic area).
Chest x-rays were rated for presence or absence of calcification in the aortic knob, and graded as grade 0 (no calcification), grade 1 (localized in the aortic arch, below the 50% girth and thickness[<2 mm]), or grade 2 (presence of multiple calcification beyond aortic knob or 50% circumference of aortic knob or heavy thickness [≥ 2 mm]) of calcification.
Patients with higher-grade calcification were more likely to be female (P = 0.16), older (P <0.001), have a history of diabetes mellitus (DM) (P <0.001), and lower highdensity lipoprotein (HDL) cholesterol level (P = 0.007). Hypertension was more frequent in the group of patients with grade 1 calcification (P <0.001).
The study showed that the higher the grade of AKC observed, the thicker the atheroma. More patients with grade 2 AKC had ≥5 mm atheroma thickness and complex atheroma (P <0.001) than did patients with lower grades of AKC.
After adjustment for age, sex, DM status, hypertension, and HDL, grade 1 AKC was associated with a 4.7-fold increase of ≥5 mm atheroma thickness (95% confidence interval [CI], 1.907-11.450) and 4.6-fold increased risk of complex atheroma (95% CI, 2.056- 10.356). Grade 2 AKC was associated with a 7.2-fold increased risk of ≥5 mm atheroma thickness (95% CI, 2.139-24.319) and a 21.1- fold increased risk of complex atheroma (95% CI, 6.312-70.797).
Epicardial Adipose Tissue: Can It Predict Metabolic Syndrome in the Elderly?
Interest has grown in the assessment of epicardial adipose tissue (EAT) because of its potential clinical association with metabolic syndrome (MetS). Previous studies have largely been conducted on a younger population (<50 years) for predicting cardiovascular risk. Researchers from Hofstra North Shore Long Island Jewish School of Medicine and St Luke’s- Roosevelt Hospital Center in New York used echocardiography to assess EAT in the elderly population (>70 years) of patients referred for echo evaluation between January 2010 and May 2012. Patients with prior cardiac surgery or pericardial disease were excluded.
EAT thickness (EAT-th) was determined in the parasternal long axis view by measuring the echo-free space between the outer RV free wall myocardium and the visceral pericardium at end-systole. MetS was determined based on clinical chart review using currently accepted NCEP ATP III guidelines.
EAT-th was measured in 101 patients (30% male; 72 ±10 years; BMI 30±8 kg/m2). Mean EAT-th was higher in patients with MetS (P = 0.008). In univariate analysis, EAT correlated with the presence of MetS, hypertension, and diabetes mellitus. In multivariate analysis, hypertension and DM correlated with EAT.
The AUC for EAT-th as a predictor of MetS was 0.67 (SE, 0.06; 95% CI, 0.54-0.79; P = 0.01), with an EAT-th cutoff of 7.6 mm, yielding a sense of 71% and spec of 56% for detecting MetS.
The study confirmed the positive correlation between EAT-th and MetS risk factors in an elderly population. The clinical relevance of the findings is not yet determined. If found at a later time, EAT could suggest an underlying metabolic disorder that would merit further investigation.
Is Pocket Ultrasound Accurate for Assessment of LV Function?
Rapid bedside assessments of cardiac function are extremely valuable in critical care settings. Pocket ultrasound devices promise high-quality 2-dimensional (2D) images at a reasonable price, ease of use, and extreme portability.
Australian doctors from Princess Alexandra Hospital in Brisbane studied 45 consecutive patients with clinically indicated transthoracic echocardiograms (TTEs) and limited 2D imaging of the LV with a pocket-sized device to assess whether these pocket devices are accurate at predicting left ventricular (LV) function. All examinations were performed by an experienced sonographer. LV function was assessed from the standard views by an experienced and novice physician and sonographer, and graded to be of normal, mild, moderate, and severe dysfunction. Presence or absence of regional wall motion abnormalities (RWMAs) were also noted.
Of the 45 patients examined, 53% were males and the median age was 60 years; all patients had images of acceptable quality. Normal LV function was seen in 68.9% of patients. Cohen’s kappa (k) showed a strong agreement between the standard and pocket devices in LV function assessed by an experienced reader (91%, k = 0.82; P <0.01)and sonographer (86%, k = 0.73; P <0.01) . Novice sonographers and readers could accurately interpret LV function 79% and 62% of the time, respectively. RWMAs were accurately detected with the pocket device.
The researchers concluded that pocket devices can be used to reliably assess LV function. “They are easy to use, with results comparable to standard equipment and little interobserver variability,” they said, and can be used effectively by novice users with a limited learning curve.
Effect of Bariatric Surgery on Cardiac Mechanics in Obese Patients
Bariatric surgery is considered a therapeutic option for morbidly obese patients, with data showing that this surgery may improve major cardiovascular morbidity and mortality. South Korean researchers, led by Sung-Hee Shin, MD, of Inha University Hospital in Seoul, assessed the changes in left ventricular (LV) mechanics after bariatric surgery in 23 obese patients. Patients had undergone Roux-en-Y gastric bypass for obesity (age = 39 ± 12 years; males:females = 6:17).
measurements were measured. LV global longitudinal, circumferential, and radial deformations were assessed using 2-dimensional speckle tracking software.
Bariatric surgery resulted in a significant weight reduction of 27.8 ± 17.5 kg over 14.7 ± 3.8
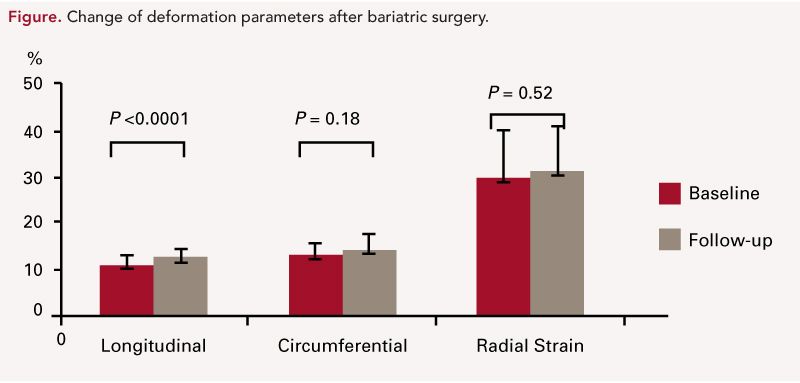
months (P <0.001). LV size and mass decreased significantly and the ratio of early-to-late diastolic mitral inflow and early diastolic tissue Doppler velocity increased postoperatively. While LV ejection fraction did not significantly change, LV longitudinal strain significantly increased after surgery. LV circumferential and radial strains were comparable at follow-up. (Figure)
The researchers concluded that in obese patients, significant weight loss by bariatric surgery led to regression of LV hypertrophy and improvement in LV longitudinal deformation and diastolic function. Therefore, they believe their findings may lend support to other data showing that bariatric surgery has beneficial effects for future cardiovascular outcomes in obese patients.
Determinant Factors of Elevated Plasma B-Type Natriuretic Peptide Level in Severe Aortic Stenosis
Elevated plasma B-type natriuretic peptide (BNP) level is a predictor of outcome and can help predict risk stratification in aortic stenosis (AS). However, progression of left ventricular (LV) diastolic dysfunction with aging may influence plasma BNP levels in elderly patients with AS. Japanese researchers led by Shunsuke Sasaki, MD, of the Sakakibara Heart Institute in Tokyo hypothesized that determinant factors for elevated plasma BNP level may be different in elderly versus younger patients with AS.
They performed echocardiography in 341 patients with severe AS (aortic valve area [AVA] <1.0 cm2), and classified them into 2 groups by age (elderly ≥75 years, n = 201; younger <75 years, n = 140). Patients with chronic renal failure and other significant valvular disease were excluded. Multivariate linear regression analysis was used to assess determinant factors for plasma BNP level separately in both groups.
Both elderly and younger patients had similar AVA indices: 0.46 ± 0.13 cm2/m2 and 0.46 ± 0.12 cm2/m2 (P = 0.06), respectively. However, elderly patients had an increased ratio of mitral peak velocity of early filling (E’) to early diastolic mitral annular velocity (E’) (E/e’) (20 ± 8 and 16 ± 6; P <0.01) compared with younger patients.
LV ejection fraction, LV mass index, E/e’, estimated systolic pulmonary artery pressure, and the presence of atrial fibrillation were found to be independent determinants of plasma BNP level in both elderly patients and younger patients.
The researchers concluded that there may be differences in determinant factors of plasma BNP level between elderly and younger patients with AS. In elderly patients with AS, plasma BNP levels may be more influenced by diastolic dysfunction rather than AS severity compared with younger patients.
Prognostic Value of Left Atrial Volume Index Change After Primary Coronary Intervention in Patients With STEMI
Left atrial volume index (LAVI) is 1 prognostic indicator for acute myocardial infarction. Values of 32.0 mL/m2 or more have been associated with poor prognosis. However, little is known about the usefulness of LAVI dynamic changes after primary coronary intervention (PCI) in patients with STelevation myocardial infarction (STEMI).
Donghan Kim, MD, and colleagues from the Republic of South Korea analyzed 244 eligible STEMI patients undergoing PCI, performing echocardiographic studies at baseline and at 12 months, with clinical follow-up at 30.8 ± 7.5 months. Patients were divided into 2 groups according to the degree of change in LAVI derived from the previous report: change in LAVI ≤2.5 mL/m2 (n = 146) and change in LAVI >2.5 mL/m2 (n = 98). The primary end point was the composite of major adverse cardiac events including death, atrial fibrillation, hospitalization on heart failure, and revascularization.
In multivariate Cox regression analysis adjusted for male gender, glomerular filtration rate (GFR), smoking, Killip class (≥III), heart rate, history of ischemic heart disease, statin use, BNP, left ventricular (LV) systolic function, LV end-diastolic dimension, LAVI, change in LAVI, stent diameter, successful PCI, follow-up LV systolic function, and diabetes mellitus, the change in LAVI >2.5 mL/ m2 group had significantly increased major adverse cardiac events (MACEs) in STEMI patients. However, there were no differences in death rates, including cardiac or noncardiac death and revascularization. Change in LAVI >2.5 mL/m2 was the independent prognostic factor of MACEs as well as GFR, and LV systolic function using ejection fraction.
Dr. Kim and colleagues concluded that in STEMI patients undergoing primary PCI, change in LAVI is a useful parameter to predict MACE, including atrial fibrillation and hospitalizations for heart failure.
Prior to surgery patients had undergone echocardiography, which was repeated at least 1 year after bariatric surgery. Parameters including tissue Doppler






