Expert Perspectives: New Treatment Options for Psoriatic Arthritis
A dive into a half-dozen promising agents for the psoriatic condition and their supporting trial data.
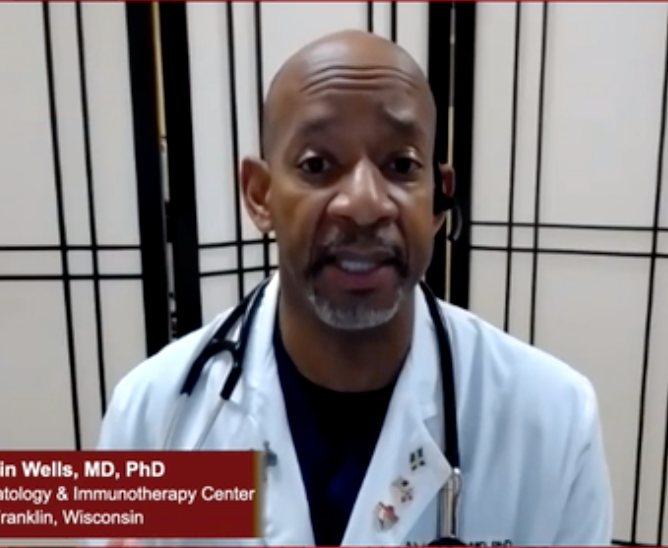
Alvin F. Wells, MD
A wide range of new treatment options for psoriatic arthritis are on the horizon, and rheumatologists got a glimpse of emerging research at the American College of Rheumatology’s virtual meeting, ACR Convergence 2020 in November.
Alvin F. Wells, MD, a rheumatologist with Aurora Health Care in Franklin, Wisconsin, shared his his insights on new treatments and how they might be applied during a webinar titled “Expert Perspectives on Management of Rheumatic Diseases: Post ACR Convergence 2020.”
The webinar was hosted by Christopher Parker, DO, a rheumatologist with The Austin Diagnostic Clinic in Texas.
Apremilast
One abstract looked at the probability of patients with active psoriatic arthritis (PsA) who haven’t taken disease-modifying anti-rheumatic drugs (DMARDs) achieving low disease activity or remission with apremilast, which is a phosphodiesterase inhibitor.
The study included DMARD-naïve patients in the PALACE 4 study and found that the likelihood of achieving low disease activity or remission at 52 weeks for those patients was higher than for DMARD-experienced patients in PALACE 1-3.
“Remember that if somebody has failed three or four different drugs, whether that’s a DMARD, methotrexate, leflunomide or sulfasalazine, when the fourth or the fifth drug comes along it’s going to be harder for them to respond,” said Wells, who is an investigator in the PALACE study.
He said evidence shows that apremilast works faster and is superior to methotrexate. However, there are some patients, for example those experiencing nausea, diarrhea, headache or depression, for whom methotrexate might be a better treatment option.
Ixekizumab
Wells also discussed a head-to-head comparison of the safety profiles of ixekizumab, which is an interleukin 17 (IL-17) inhibitor, and adalimumab, which is a tumor necrosis factor (TNF) blocker, at 52 weeks. Ixekizumab was shown to be superior to adalimumab for improving joint and skin disease. The study found that there were more severe adverse events among patients in the adalimumab group (12% vs 4.2%; P <.001).
“It showed that on ixekizumab there’s a little bit more injection site reactions and a few patients had some exacerbation of underlying inflammatory bowel disease that you don’t see in patients on adalimumab,” Wells said.
He suggested monitoring fecal calprotectin levels to tell if someone has a subclinical inflammatory bowel disease before administering the drug, which could be billed under high-risk medical monitoring.
“I’m not quite there yet,” he said. “But just like we make sure somebody’s screened for hepatitis B, make sure we give somebody the varicella vaccine, all those things before starting these drugs, that might be what I’m thinking about before starting an IL-17 drug.”
Tofacitinib
Tofacitinib, which is a Janus kinases (JAK) inhibitor in pill form, was evaluated for efficacy in improving dactylitis.
“The take-home message is the data showed that it worked and the safety profile was comparable to what we’ve seen in all the other RA studies with this drug,” Wells said.
He said monitoring what he called a sentinel joint with a lesion larger than 2 centimeters can help determine whether the drug is effective or if trying a different medication is in order.
Wells described what he called the “triple ripple” of indicators, including clinical signs, biomarkers and imaging, to determine whether a patient is in complete remission before determining whether to ramp up or back off medication.
“We use all those different tools,” Wells said. “We really want to talk about complete remission. It’s a clinical remission, no tender joints and swollen joints; it’s a biomarker remission, so normal sed rate and CRP; and the other one is an imaging remission, no activity on the ultrasound signal. That’s what we look for.”
Upadacitinib
For patients with an inadequate response to biologic DMARDs, upadacitinib was evaluated for safety and efficacy in a double-blind, randomized controlled Phase 3 trial. The study showed significant improvements in joint and skin signs and symptoms.
Wells said it makes sense scientifically that a drug like upadacitinib could provide efficacy where a more targeted biologic fell short.
“When you give a biologic drug, that’s like somebody coming in here and turning off the light switch,” Wells said. “It’s going to stay dark until the light switch comes back on, until the half-life goes away. The difference with the JAK inhibitors when you give them they hit 12 different pathways, but guess what? It doesn’t turn the light switch off on all of them. It dims the lights just enough to get the disease under control.”
Deucravacitinib
Deucravacitinib is a novel agent that inhibits Tyrosine kinase 2 (TYK2). The study showed that at week 16, 52.9% of patients taking 6 mg deucravacitinib and 62.7% of those taking a 12 mg dose reported improvements. No serious side effects were reported.
“We are now with PsA treatment options where we were with rheumatoid arthritis several years ago,” Wells said. “Every six months or every year we’re seeing new data with new targets to treat the disease. Why is that? Because we haven’t hit the holy grail.”
More research is needed to evaluate the drug’s safety and effects on bone marrow and viral infections.
Neihulizumab
Another novel treatment, neihulizumab, is a monoclonal antibody that binds to CD162, one of the CD markers on the surface of a T-cell. The study showed the treatment was well tolerated and may have clinical utility.
“It increases natural cell death,” Wells said. “It increases T-cell apoptosis. It’s very selective, doesn’t hit the B-cells, doesn’t hit the macrophages. So, the question is, in patients with active psoriatic arthritic can we target the T-cells? This shows that yes, we need to see that.”
Wells said that while early trials suggest it might work, he’s concerned about the potential for viral infections and more research is needed.